Studies Actively Recruiting

Functional Near-Infrared Spectroscopy (fNIRS) to Assess Brain Activity in Children and Adults with Movement Disorders
Neural imaging during movement has become more portable by utilizing an approach termed functional near-infrared spectroscopy (aNIRS) as a means to isolate areas of brain activity. fNIRS is a non-invasive imaging technology that uses low levels of nonionizing red and near-infrared colored light to measure the hemodynamic state of the brain. Although use of these technologies for assessing cortical activation patterns is increasing, validation of these approaches, particularly in children and those with brain injuries such as cerebral palsy, is in the early stages. In this protocol, our objective is to systematically compare cortical activation patterns associated with specified motor and sensory tasks in healthy children and adults to those with unilateral or bilateral childhood-onset neurological injury. The results of this study are expected to increase knowledge of brain activation patterns across tasks and groups with and without brain injuries and to provide for future clinical studies with these technologies.
Rigid Body Database
The purpose of this study is to utilize motion capture technology to accurately and precisely quantifying the different ways people control limb and whole body movements. This information will be used to develop a database on normal movements and adaptive movements of people who have diseases that affect the way they move. The database will serve as a tool to improve diagnosis and treatment of patients with movement-related problems. Electrical activity in the muscles also may be measured, using small metal electrodes attached to the surface of the skin with an adhesive bandage.
Promoting Upright Mobility in Infants with Cerebral Palsy Using a Robotic Unweighting System
The objective of this study is to quantify the effects of mobility training with a motorized unweighting system (BabyG) to improve crawling and walking abilities in infants diagnosed with or at high risk for Cerebral Palsy (CP). Infants ages 4 months to 18 months with or at high risk for CP who are not yet walking independently are eligible for this study. The protocol consists of 12 weeks of mobility training with a motorized unweighting system (BabyG). Infants will come for 2-3 visits per week at the NIH clinical center. They will be encouraged to crawl, walk, and play in the harness during each training session. We will perform assessments of brain activity and motor development before and after training.

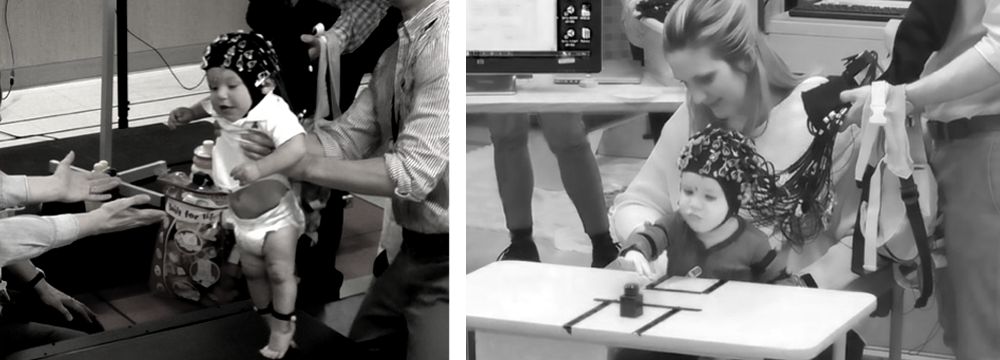
Near-infrared Spectroscopy and Electroencephalography to Assess Cortical Activation During Motor Tasks in Infants and Toddlers with or at high-risk for Cerebral Palsy
The purpose of this study is to investigate how infants’ brains change as they learn new motor skills. Infants aged 3 months and up with and without cerebral palsy (CP) who are not yet walking independently are eligible for this study. Results may assist with better treatment methods for CP. You and your child will come for 2 or more visits at the NIH Clinical Center. The visits will last approximately 2-3 hours. Your infant will wear a snug cap containing electroencephalography (EEG) sensors that record brain activity. They will be encouraged to reach for toys and to take supported steps on a treadmill.