Patient with rare spinal cord cancer bounces back
After being diagnosed with a rare cancer in her spinal cord, 38-year-old Sarah Rosenfeld looked to the NIH for help. At the Clinical Center, researchers are studying more than 500 rare diseases in partnership with nearly 15,300 unique patients like Rosenfeld.
In January 2016, Rosenfeld, began to experience intense pain in her lower back and leg. After numerous doctors' visits, her medical team in Northern Virginia finally found the cause. Her MRI results showed a myxopapillary ependymoma, or slow-growing tumor, in the lower portion of her spine. The tumor, which was 5 centimeters (about the size of a lime) arises from the supportive tissue of the brain and spinal cord.
This type of cancer can often be cured by surgically removing the tumor. But for Rosenfeld, that was not the case. In April, her medical team was unable to remove all of the tumor.
"Hearing a diagnosis of cancer is frightening, but you have to let go of the fear and get started asking lots of questions," Rosenfeld said. "The doctors advised me to wait and have the remaining tumor monitored, but I wanted to take a more proactive approach."
That's when she heard of the NIH. One of Rosenfeld's neurosurgeons explained to her that the Clinical Center may be able to provide treatment opportunities for the tumor in her spinal cord.
"Myxopapillary ependymoma is a rare tumor so it was essential that I found somewhere that had experience treating it. Learning about the clinical trials at NIH was fortuitous," Rosenfeld said. "All the brilliant minds for this are here. I feel very fortunate and lucky to be a patient."
More information on myxopapillary ependymoma
Ependymal cells form a lining around cerebrospinal fluid structures inside the brain, spinal cord, and filum terminale (a fiber at the lower end of the spinal cord). Ependymoma is a tumor of ependymal cells, which arises when unregulated division of ependymal cells creates a mass of cells, which recruits a blood supply which sustains further cell division and tumor growth. A myxopapillary ependyma grows from ependymal cells in the filum terminale, and is called myxopapillary because of Greek and Latin words, "myxo" meaning mucus and "papillary" meaning exhibiting projections. When a thin slice of a myxopapillary ependymoma is view under the microscope, one observes thick mucus (myxo) and blood vessels surrounded by finger-like projections of cells (papilla).
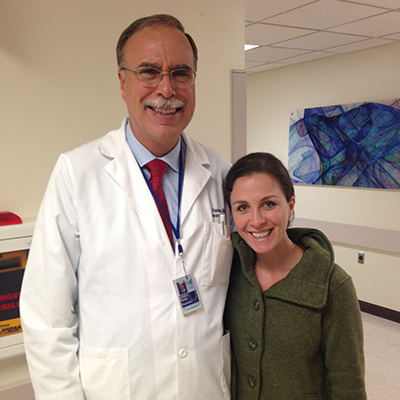
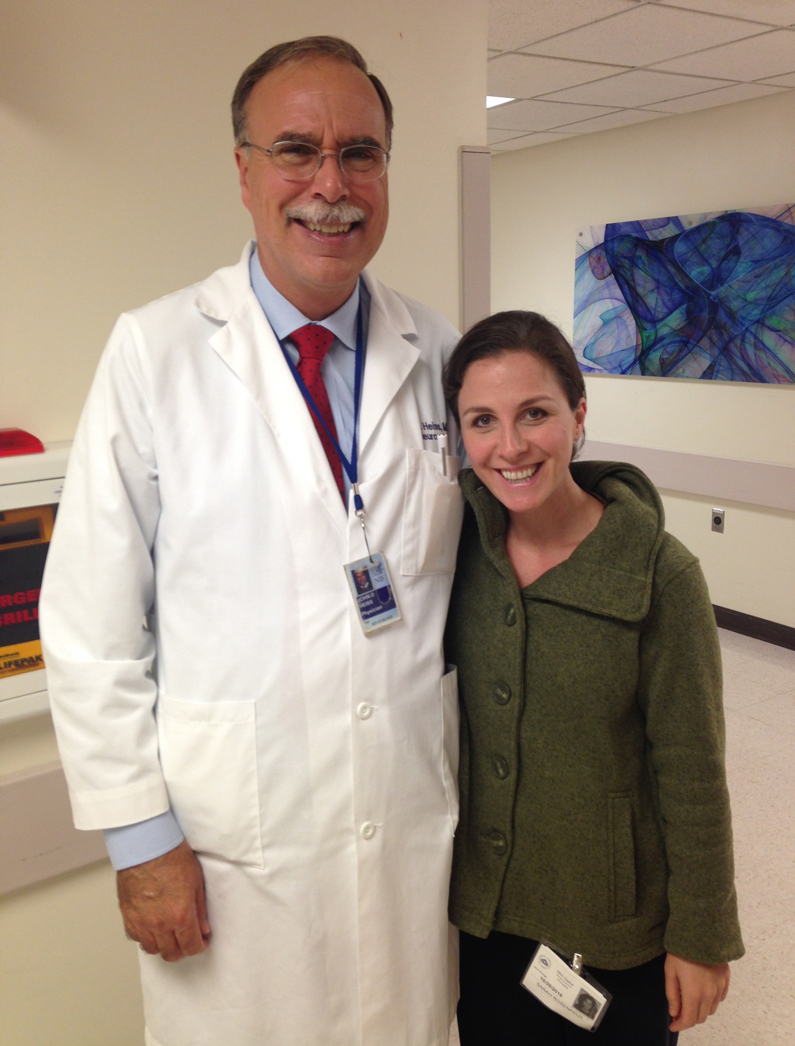
- Dr. John Heiss, Surgical Neurology Branch of the National Institute of Neurological Disorders and Stroke (NINDS)
Three months after her first surgery, she came to the Clinical Center and met with Dr. John Heiss, with the Surgical Neurology Branch of the National Institute of Neurological Disorders and Stroke (NINDS).
Heiss is part of a NIH multi-institute neuro-oncology team that includes physicians and scientists with a shared mission of providing cutting-edge treatments and research studies to patients with brain and spinal tumors. The multispecialty team includes neurosurgeons, neuro-oncologists, neuroradiologists, neuropathologists, radiotherapists, nurse practitioners, research nurses and scientists.
Together, Heiss and Rosenfeld reviewed a new MRI of her spinal cord which revealed residual tumor tissue.
Heiss and his team recommended a second surgery followed by radiation. In October 2016, Heiss and many others colleagues conducted a nine-hour procedure in the operating room to try to remove the tumor tissue. Doctors were able to remove nearly all of the remaining tumor tissue except for a small amount that, due to its placement, was deemed too risky to remove surgically. The possibility of causing permanent nerve damage was too great.
The NIH team decided the next step was to irradiate the remaining tumor cells. This involved 30 treatments over six weeks — once a day every day except for weekends and holidays.
The nurses and support staff at the hospital were instrumental in getting her through the process, she said. The radiation itself was not painful but the aftermath for Rosenfeld was fatigue, among other side effects.

"[Our] team includes some of the world's experts in ependymoma therapy, outcomes and research," Heiss said. "Brain and spinal tumor specimens removed at surgery by NINDS neurosurgeons undergo histopathological analysis and molecular profiling to identify tumor characteristics that make them susceptible to specific treatments. NIH clinical and laboratory research on ependymoma and other malignancies has the ultimate goal of improving the care and long-term outcomes of patients."
"They were so supportive and understanding," Rosenfeld said. "The level of patient care here is like nowhere else. On my last day of treatment, (the staff) gave me flowers, an NIH sweatshirt and a card. I was thrilled to be finished with radiation, but quite sad to say goodbye to everyone."
"It is a very patient-centric environment here," said Lois Goodstein, her mother. "You draw comfort and hope knowing that you are at the absolute best place for this."
Rosenfeld will continue to be monitored and scanned at the NIH for at least the next year. She is participating in three clinical trials at the Clinical Center: Evaluation and treatment of neurosurgical disorders 03-N-0164; Care of the adult oncology patient 04-C-0165; Evaluation of the natural history of and specimen banking for patients with tumors of the central nervous system 16-C-0151.