Content on this webpage is provided for historical information about the NIH Clinical Center. Content is not updated after the listed publication date and may include information about programs or activities that have since been discontinued.
Keith Sargent came into the Rehabilitation Medicine Department’s foot clinic hobbling painfully on partially amputated feet. Before he left, he was running in the hallway.
“This feels great! I don’t feel any more pain. I have no pain,” said Sargent.
Sargent is just one of hundreds of patients who have come to the foot clinic with one last ounce of hope that their foot problems will finally be solved by this 10-member team of doctors.
This year, the clinic celebrates 15 years of service.
The foot clinic has become the last resort for patients with complicated foot problems that have been consistently treated by podiatrists and surgeons without success. When all treatments have been exhausted, the patients are then referred to Dr. Lynn Gerber and the foot clinic.
“We are determined to improve our patients function,” said Dr. Gerber, chief of the Rehabilitation Medicine Department.
Dr. Gerber heads up the foot clinic and has been a part of it since its inception in 1986. “We challenge ourselves. We try our best to avoid sending our patients out without helping them. We don’t like to say ‘You deal with this.’”
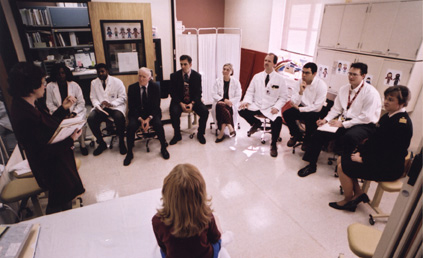
Each of the 10 doctors represents a different podiatric discipline that includes physical medicine, physical therapy, pedorthists, biomechanists, podiatrists, orthopedists and students.
During a session, the doctors interview one patient, analyze the problems, and brainstorm ideas among themselves to come up with the best remedy.
“You will never find ten professionals in a room spending time with one patient anywhere,” said Karen Lohmann Siegel, physical therapist with the Rehabilitation Medicine Department and a member of the foot clinic.
The clinic meets twice a month for about two hours and examines one to four patients each session.
According to Gerber, the patients continue to attend sessions until they have shown improvement and are able to return to normal activities. For Sargent, returning to normal activity is his ultimate goal.
“My first priority is to walk better than before, then move on to hiking, then skiing,” said Sargent.
Five years ago Sargent was cycling home when an accident caused his bike to go off the road and into a river. The accident left him disoriented and stranded in frozen water.
Now Sargent stuffs the front of his shoes with tissues to fill out the area his toes and part of his foot would occupy if frostbite had not caused them to be amputated. The rest of his shoes are packed with gel and foam pads, which have been futile in helping him return to his active lifestyle.

“This is the most positive experience I’ve ever had with doctors,” said Sargent, who received a temporary, custom-made orthotic to replace the patchwork of foam pads and gels inserted in his shoes.
Sargent waited two hours as Chris Gracey and Joe Shrader, physical therapists with the Rehabilitation Medicine Department, constructed the orthotic and allowed Sargent to try it out. Sargent to try it out. Based on Sargent’s suggestions, Gracey and Shrader sanded and glued until it was a perfect fit.
“I feel fortunate that they aren’t running off to one hundred other patients,” said Sargent. “It’s like complete, customized service.”
Sargent will soon be the recipient of a new device called the Oregon Brace System that will allow him to walk better and ultimately return to regular activities.
Nancy Griffin also knows how painful feet can halt normal activities. Last April, Griffin had three screws placed in her right foot to hold it together after arthritis wore away the joints. But since the surgery, Griffin’s foot has remained red and swollen.
“I think the surgeon screwed the screws in too tight,” she joked as she showed the team of doctors her foot.
She can’t walk on flat surfaces and has to wear flip-flops in the shower just to be able to stand. She has gone through a variety of braces and boots to ease the pain and help her walk, but all have been unsuccessful until now.
“You don’t know how relieved I am to have all of those fine minds to help me find a way to walk and be productive,” said Griffin. “I have hope again.”
She has hope because “a lot of physicians deal with management, not function,” said Dr. Galen Joe, senior staff fellow with the Rehabilitation Medicine Department. “We focus on function and day-to-day living.”
—by Tanya Brown

