The Clinical Center’s new Pain and Palliative Care Consult Service opened in August and already boasts more than 100 patients. The service uses a multidisciplinary approach to manage patient’s pain, and the associated symptoms.
“Our multidisciplinary team helps to address the quality of life, pain, and symptom management issues outside of a patient’s protocol,” said Dr. Ann Berger, chief of the CC Pain and Palliative Care Consult Service. “This approach helps to treat the whole person and makes them feel better.”
Patients are referred to the service by their physicians, and after an initial assessment, team members from various CC departments collaborate on the best approach.
“We begin by looking at pain and how it affects a patient’s emotional state, and other symptoms,” said Dr. Berger. “That way when we bring our team together we can work to pinpoint critical areas of care.”
Dr. Berger, a former oncology clinical nurse specialist who received medical training at the Medical College of Ohio, initiated palliative care services at both Yale University, and Cooper Hospital/University of Medicine and Dentistry in New Jersey, before joining the CC.
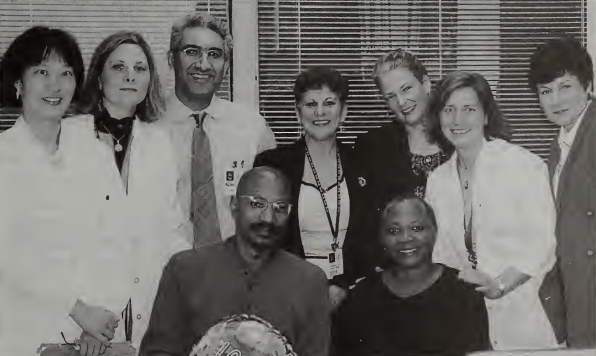
The core staff of the service includes Dr. Berger and nurse practitioners Donna Pereira and Karen Baker. The multidisciplinary team includes representatives from rehabilitation medicine, pharmacy, nutrition, anesthesia, spiritual ministry, social work, bioethics, and the CC patient representative.
According to Dr. Berger, educating health professionals in the field of pain and palliative care has increasingly received more emphasis in recent years. The American Medical Association has initiated a program to educate physicians on how to provide pain and palliative care, and questions can now be found on the internal medicine board exams.
“The JCAHO made pain a fifth vital sign for its accreditation process,” said Dr. Berger. “This shows that pain and palliative care is a growing field in the country.”
But education, says Dr. Berger, is a critical component. The staff has already initiated training for the multidisciplinary team and looks towards providing specialized training for the medical and nursing staff on each patient-care unit.
“It is critical for staff to understand and identify the possible components of one’s pain experience so that appropriate treatments can be implemented,” said Dr. Jay P. Shah, a physiatrist in the Rehabilitation Medicine Department and a collaborator in the service.
“We are integrating nonpharmacologic treatments, such as those we use in physical medicine and rehabilitation, with pharmacologic management,” said Dr. Shah. “It’s a pyramid strategy: first we try to manage pain with physical and psychosocial modalities, and then introduce drugs as needed. Many patients have benefited tremendously.”
Timing is everything when it comes to these issues, say the program planners.
“We are here for patients from day one of their illness, not only for end-of-life issues,” said Dr. Berger.
Patients who are experiencing anything from fear and anxiety, to nausea and vomiting are encouraged to participate in the service.
“It’s a patient's quality of life that makes all the difference. We not only have to cure the illness, we have to take care of the person,” said Dr. Berger. “More and more patients are saying that they want both. That is our purpose, to give them both.”
Outpatient clinics are held Mondays and Thursdays in OP3. Inpatients are seen all week. For more information, call 4-9767.
—by LaTonya Kittles

