Clinical Center News
Cimino shares BTRIS vision at CC forum
 |
|
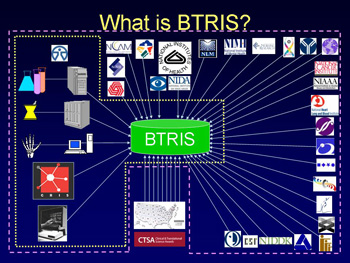
This slide from a town hall meeting presentation given by Dr. James Cimino, chief of the new Laboratory for Informatics Development, visually represents the multiple sources of data for BTRIS, the Biomedical Translational Research Information System.
|
Dr. James Cimino, chief of the new Laboratory for Informatics Development, at a Clinical Center town hall meeting on Feb. 26 presented his vision for BTRIS, the Biomedical Translational Research Information System. It will be a new resource that investigators can use to help identify promising new avenues for research and foster data-sharing across institutes and with extramural collaborators.
Cimino comes to NIH from Columbia University, where he was a professor of biomedical informatics and medicine. The data repository he helped develop at Columbia will be a prototype for NIH’s BTRIS, but with some very important distinctions. First, Columbia’s project reused clinical patient data for research and patient care; it was not collected as part of a research protocol. Second, BTRIS will be a next generation system—Columbia’s began in 1988—and will more easily integrate 21st century features such as images and genomic data. Finally, BTRIS is an opportunity for NIH to create a centralized repository aggregating and standardizing data currently isolated in disparate systems.
Cimino is seeking volunteers—those who think they are very likely to use and benefit from BTRIS—to participate in his principal investigator user group. It’s a weekly commitment to meet, help set requirements and priorities for BTRIS, serve as beta testers, and receive the first access to the BTRIS demonstration project, which is expected in July 2008. The rest of the CC will be introduced to BTRIS version 1.0 in July 2009.
 |
|
Dr. James Cimino presenting at the CC town hall meeting about his vision for BTRIS.
|
In addition to the PI user group, Cimino will also meet regularly with a policy working group to address the ethical, legal, and human subjects research issues raised by the project. The application of biomedical research data to providing patient care, also known as translational research, will address confidentiality and data access issues with the flow of data in and out of BTRIS at stages such as deidentifying and reidentifying data, aggregating data over time, converting data to relevant concepts, and identifying relationships across data and correlations to test hypothesis.
“If someone asks, ‘Will BTRIS include this type of data?,’ the answer is always yes. We want to include all clinical and non-clinical data that our partners are willing to share with us and allow broader data access,” Cimino said. Each data element will have requirements for access to assure absolute compliance with policies. Analysts will also help staff run more complex queries, as well as provide training and tutorials on how to use BTRIS.
A videocast of the town hall meeting is archived at http://videocast.nih.gov/Summary.asp?File=14320. For questions or comments about BTRIS, contact Cimino at ciminoj@cc.nih.gov.
Back to Top
CC volunteers find bridge to medicine
 |
|
(from left): Dr. Cynthia Guime-Gonzalez and Vanessa Flores, who have both volunteered as CC Spanish language interpreters as they progress in their medical careers.
|
Each year, the Clinical Center Social Work Department honors volunteers during National Volunteers Week, April 27 to May 3. Sponsored by the Points of Light Foundation, the week thanks one of America’s most valuable assets, our volunteers, and calls attention to all that they do to improve our communities.
CC volunteers often find their time here to be a meaningful experience that enriches their personal and professional lives. For Dr. Cynthia Guime-Gonzalez and Vanessa Flores, who both began as volunteer Spanish language interpreters, their work at the CC contributed to their path to becoming physicians and establishing their medical practices.
A U.S. citizen who moved to Panama at a young age, Guime-Gonzalez has volunteered at NIH since 1998 during her vacations to visit relatives in Bethesda. She earned her medical degree in Panama this spring and returned to the U.S. to practice what she learned there. After she finishes studying for her boards, she will apply for a U.S. residency program, possibly in oncology. Guime-Gonzalez often attends rounds in the CC and enjoys visiting with oncology physicians and patients to understand the differences between care provided in the U.S. at NIH and Panama.
Originally from Guayaquil, Ecuador, Flores in 2007 completed her third summer program at NIH as a research student with the NHLBI’s vascular medicine branch. She also worked with NIMH in the summer of 2005 and interned in the Social Work Department’s volunteer office in 2004.
During Flores’ senior year of high school, she heard from an anatomy and physiology professor how countries like the United States support scientists who spend a lifetime on finding alternatives in medicine and cures for rare diseases. “This was a huge inspiration to me, so I packed my belongings, immigrated to the U.S., and pursued opportunities in medicine with a biomedical research track.” Flores’ search brought her to the CC, where she was excited to see how translational medicine works. “You don’t usually see the beginnings, the initial questions that lead to innovation, but all those things must occur to develop and bring new therapies to the world,” Flores said. “Coming to NIH gave me that perspective and also raised my awareness about public health issues. I want to collaborate with research institutions and be a part of the evolution of improving medicine.”
Flores is a participant in the NIH Undergraduate Scholarship Program, which offers competitive scholarships to students from disadvantaged backgrounds who are committed to biomedical, behavioral, and social science health-related research careers. She will return to NIH to serve one year of full-time employment for each year of scholarship tuition she receives to attend a combined M.D. and master’s program in clinical research at the University of Pittsburgh’s School of Medicine. Flores says she hopes to become a physician with expertise in clinical research who fosters translational medicine and contributes to the improvement of quality of life for individuals and communities.
The never-ending, ever-changing challenges of a medical environment hooked both women. Flores used the flu as her example. “It’s different every year, and the patients don’t always react the same way. You’ll never have the perfect technology, antidote, or procedure as people are constantly evolving. There’s always something new to work on to move all of medicine forward. There’s always something I can do or contribute by applying my determination and intelligence toward looking for answers for the good of society,” she said.
 |
|
Dr. Cynthia Guime-Gonzalez with German, a former patient in Panama who continues to inspire her.
|
Guime-Gonzalez knows what keeps her going when she encounters challenges in her path to practicing medicine. While completing her pediatric rotations in 2005 at Hospital Del Nino, a public children’s hospital in Panama, Guime-Gonzalez met German, a nine-year-old boy who had one leg amputated to prevent the spread of cancer in his femur. The first day Guime-Gonzalez talked to German, he was excited and talkative. The second day he was quieter, and Guime-Gonzalez forgot to check his chart before approaching him. “He seemed like a 90 year-old boy,” Guime-Gonzalez remembers. “He said, ‘Didn’t they tell you that I’m going to die? I know everything will be fine for me, but I’m sad because I know my family will suffer.’”
German died about a week after Guime-Gonzalez met him, but not before teaching her so many things, especially how physicians can think they’re going to provide encouragement to their patients, but end up drawing encouragement from them instead. German was part of a local foundation helping kids with cancer, and he would say that he knew God wanted to take him now, but he wanted the doctors to find something to help his friends in the foundation. “ German told me, ‘I know you will find something someday to cure this.’ Whenever I struggle or am scared, I remember his statement,” Guime-Gonzalez said.
The diversity of patients and people found at NIH also impressed them both. Flores recalled how growing up, she only met Ecuadorians, but discovered a melting pot of cultures at NIH. She recalled in particular a low-income Bolivian CC patient, whom she gave some Spanish language brochures about her protocol. “I saw that she was frustrated and figured out that she didn’t know how to read. That reminded me to stay attuned to the people I encounter in this building. Not everyone can do everything, whether it’s reading, writing, walking, eating, or showering—all those things we take for granted. A simple task, like making an appointment with a nurse, isn’t an easy task for some patients. A more common day-to-day task in their typical environment might be feeding their chickens or packing goods on their mule to sell in the town.”
 |
|
(from left): Dr. Cynthia Guime-Gonzalez and Vanessa Flores discuss their experiences as CC volunteers.
|
Flores and Guime-Gonzalez challenged CC and NIH staff to continue to engage patients from different cultures with tact and compassion. “As an international organization, a global knowledge center, CC and NIH staff should continuously globalize their minds as well,” said Flores. “You’re serving everyone you’re working with and for. Coming to the hospital is a big deal already for patients, they’re scared and sick. It means so much when staff take the time to reassure patients and let them know they can stay calm while they sort things out.”
Because the CC is a special hospital, with patients coming here to participate in research, the personalities of the staff are also special, according to Guime-Gonzalez. “They’re friendlier, not rushed, and they take the time to explain things. They understand that most of the information about a disease comes from the patient, so people here listen to what patients say and feel so they can provide the best treatment. I really admire the NIH staff at all levels. It feels like a big family here.”
Back to Top
'It changed my perspective about what you really need to live'
 |
|
CC nurse consultant Cynthia Herringa and her granddaughter Demi care for a baby during a clinic in the city dump of Managua, Nicaragua.
|
Cynthia Herringa, nurse consultant for the Office of Recruitment Outreach Orientation and Retention in the Department of Nursing and Patient Care Services, has traveled every January for the past five years with her church as part of a medical mission team to Nicaragua. The team conducts medical clinics in the country’s capital of Managua, local villages, and the rain forest. The team of 10-15 volunteers—including three physicians, four nurses, a dentist, and a pharmacist—commit to spending about 12 days abroad and paying for their own travel expenses, lodging, and meals. The group purchases, collects, packages, and transports medications for the trip.
Herringa said the needs she sees in Nicaragua, which after Haiti is the poorest country in the Western Hemisphere, motivate her to return every year. Although Nicaraguan national health clinics exist, they’re inaccessible to citizens both geographically and economically. Families can’t afford to buy food, let alone medications, so often common, chronic illnesses don’t receive treatment, according to Herringa. The country has high rates of infant mortality and malnutrition, no running water, and squalid living conditions.
When Herringa’s team arrives, a minimum of 250 people are waiting in line without food, water, or shelter in temperatures of more than 100 degrees to receive care at the clinic. Aside from dental extractions, no surgeries are performed, but other complaints similar to those at an urgent care clinic or general practitioner’s office are treated.
The most interesting clinic for her is the one the group holds in the city dump, where about 3,000 people live, including some children who do not know who their parents are or how old they are. “The first year, I cried for days when I came back, I had culture shock. It changed my perspective about what you really need to live.” Her enthusiasm for the mission work spread to her family: Her husband Len, who is a retired crime scene investigator from the Washington, D.C., police department, goes with her to do laboratory work. Her granddaughter Demi used her Spanish skills to help the group triage patients in Nicaragua when she was as a high school senior.
After her repeated visits, Herringa often reconnects with patients she’s seen during past trips. Young women who received her prenatal care often return to introduce their infants. One gratifying moment came last year, when a woman came up to Herringa asking if she remembered her. With no blood pressure medicines available, Herringa taught her lifestyle changes to lower her blood pressure. The woman asked her to again measure her blood pressure, which was low, and said proudly, “I did everything you told me to do.”
Although many people working at NIH know that they are helping to improve human health, volunteering on a medical mission abroad brings a different type of fulfillment. For Herringa, knowing that she is helping to meet the direct medical needs of many in the world motivated her to also help closer to home at a medical clinic in Germantown as an approved outside activity. She spends five hours each week at the clinic, which provides free primary health care and medications to uninsured low-income adults in Montgomery County. “My husband tells me that I’m always in the best mood on the days that I volunteer at the clinic. It gets you involved in something outside the sphere of your work and family.”
Photos of Herringa on her visits decorate her CC office and provide her colleagues with insights into other sides of her personality. As Herringa doesn’t have direct patient care and has worked in management for most of her career, her coworkers are surprised to see pictures of her in scrubs or playing soccer with kids. Herringa encouraged other CC staff to consider volunteering in a way that shares their expertise, whether it’s medical training or a language skill, in the local community or around the globe. “There’s so much talent here.”
Back to Top
Community caring: A three-part look at the NIH-Cardozo program
 |
|
(from left): Dr. Migdalia Rivera-Goba, CC senior nurse specialist, and Dr. Gwenyth Wallen, chief of the Research and Practice Development Service within CC Nursing and Patient Care Services.
|
by Jenny Haliski
For NIH to conduct representative clinical research, studies need to include a range of diverse participants in the investigation to gain the broadest perspective on human health. At the same time, many people in minority communities in NIH’s own backyard lack access to resources that would help them to participate in research and that many of us on campus take for granted: information, health care, transportation, and medical advocates and specialists who speak our language. Out of this mutual need, a fruitful relationship between NIH and the Washington, D.C., Cardozo community sprouted and is flourishing.
In 2000 NIAMS, under the leadership of Dr. Stephen Katz and in an effort to facilitate research on health disparities in rheumatic diseases, established a community partnership, the Health Partnership Program (HPP). The HPP includes about 68 community partners representing various sectors of the African American and Latino communities within Washington, D.C. Its guiding principles include openness about its plans and actions, inclusiveness of all constituents in partnership activities, and responsiveness to community needs and concerns, as well as those of NIH. The community is involved in both program development and the NIH research agenda, and a core group meets regularly to provide advice about outreach, research, and education activities, as well as to review research proposals.
 |
The front door to the Upper Cardozo Neighborhood Health Center, where the NIH-Cardozo clinic is located.
|
According to Dr. Barbara Mittleman, former NIAMS director of scientific interchange and current director of the Office of Science Policy’s public-private partnership program, the idea for the NIH-Cardozo relationship came in 2000. The idea of an ongoing NIH research clinic tied to on-campus research activities with movement of patients and staff between locations was quite novel at the time, she said. Unlike volunteer medical activities in local clinics, which physicians and fellows often seek out to keep up and sharpen their skills, staff at NIAMS’ CHC would be conducting official NIH duties. “The clinic was the result of everyone’s desire to do the right thing and make it happen,” Mittleman said, noting that she met biweekly for at least a year with Clinical Center department directors to set things up in a way that served patients, staff, the Cardozo community, and NIH research needs all at the same time. In addition, all aspects of NIAMS—intramural, extramural, and the director’s office—all worked together. “We had to have an interdisciplinary, multicultural
research team, with every participant adding their unique talents to the mix, for this to succeed,” Mittleman said.
 |
The entrance to the NIAMS Community Health Center
|
A major component of the HPP was the establishment of the NIAMS Community Health Center (CHC), an outreach site located within the Upper Cardozo Health Center, which is operated by Unity Health Care Inc., a nonprofit organization providing health care to uninsured and underinsured D.C. residents. The CHC provides a venue for community- based research on clinical aspects of rheumatic diseases, health education programs, and training for NIH staff. Located in the historically African American Shaw/Cardozo neighborhood, CHC’s patient population is equally divided between African American and Latino patients. “If we only studied the people showing up at the CC, we’d never be able to study health disparities. We had to go out into the community to get the participants,” Mittleman said.
Cardozo’s partners in both the Hispanic and African American communities embraced the CHC. Jesus Lopez with the United Planning Organization said his group has been involved since the clinic opened. “It offers comprehensive services to benefit people who suffer from arthritis and other health conditions. By accepting and including people from diverse racial and ethnic backgrounds, and by maintaining a high standard of professionalism, the clinic plays a key role in our community’s success.”
Nurse researchers at the CC play pivotal roles as primary and associate investigators on interdisciplinary teams of researchers, clinicians, public health policy advocates, and members of diverse communities to conduct health behavior and health disparities research. Dr. Gwenyth Wallen, chief of the Research and Practice Development Service, and Dr. Migdalia Rivera-Goba, CC senior nurse specialist within CC Nursing and Patient Care Services, forged a partnership with NIAMS nurses, physicians, and health educators and the Upper Cardozo Health Center. Health disparities is a very complicated topic involving the interplay of biology, life choices, access to care, environmental exposures, genetics, diet, economic resources, and systemic health system issues. It’s hard to tease out what elements are affecting health outcomes, according to Mittleman.
The establishment of NIAMS’ CHC provided an opportunity for the CC departments of bioethics and nursing to learn more about the views of the center’s research participants and community members regarding the ethics of clinical research. First they had to build a bridge to the community through education: giving presentations at churches, bringing researchers to speak to the community without scientific jargon, and describing the importance of participating in research. “Recruitment is fundamentally about education,” said Mittleman. “If people don’t know why it is to their benefit to participate in clinical research, you can’t recruit them, no matter how easy it is to get on campus.” Carrington said that having the medical research staff willing and ready to talk with the community was key to engaging patient interest in research studies.
 |
|
(from left): Kelli Carrington, former NIAMS outreach coordinator and current coordinator for the NIH Director's Council of Public Representatives, and Dr. Barbara Mittleman, former NIAMS director of scientific interchange and current director of the Office of Science Policy's public-private partnership program.
|
In September 2004 they held a consultation with representative members of the community. A report summarizing the results of that discussion was published in the American Journal of Public Health by Dr. Christine Grady, head of the Section on Human Subjects Research in the CC Department of Bioethics; Wallen; Rivera-Goba; Kelli Carrington, former NIAMS outreach coordinator and current OD coordinator for the NIH Director’s Council of Public Representatives; and Mittleman. Grady and colleagues presented HPP partners with three research case examples designed to stimulate discussion regarding the ethics of conducting research among individuals with limited health care access. They learned establishing and maintaining open and honest communication is a key strategy for creating trust within the community before, during, and after a study. Community members requested clear plans for follow-up care or referral so that participants would not feel used or exploited once a study ended. Familiarity with the community’s language, customs, and values were also important. Overall, the partners believed that their participation in respectfully conducted clinical research was valuable.
One of the first protocols conducted with Cardozo directly benefited its members, as well as NIH, by increasing both groups’ understanding of the health behaviors and beliefs of minority patients with rheumatic disease. Rheumatic conditions are among the most common health problems in the U.S., and there are marked differences in the incidence, prevalence, severity, processes of care, and health outcomes among racial and ethnic groups compared to white Americans. Although the effects of the disease may be modifiable by lifestyle changes, such strategies are often difficult for patients to accomplish and may be ineffective in minority communities because of differences in culture and environment and the lack of culturally sensitive materials and approaches. Wallen and Rivera-Goba conducted a protocol exploring how health beliefs and behaviors may contribute to health disparities. The part involving patients is over, and they are analyzing the data they collected, but the Cardozo community invited them to complete another clinical trial in the future. Wallen and Rivera-Goba hope to apply what they learned about what works best within the community by conducting an intervention study focusing on nutrition, physical education, and social support.
 |
|
A mural in the Cardozo/Shaw neighborhood painted by participants in the 2001 summer youth program sponsored by the Latin American Youth Center, an HPP partner since 2000.
|
“It’s all about trust when you’re working in the community,” Wallen said. “The community told us, ‘Don’t just come here to gather the information you want and leave. Come back and feed something positive back into the community with what you’ve learned.” Sometimes the giving back involves teaching, other times it involves providing access to health care treatments and medications that wouldn’t otherwise be available. The result is a win-win for both sides. “The NIH-Cardozo relationship helps to improve the health status and quality of life for the community residents. Researchers receive insights into a population that otherwise would not have the option to participate in clinical trials. They’re not on the Internet researching their conditions or able to get in a car and drive to campus,” Wallen said.
In addition to honoring the collaboration of individuals, the research program includes training and mentoring between researchers to prepare the next person for their training. Each study provides new realities about approaches to research in diverse communities and the life realities of the patients served. Rivera-Goba said, “People want to be recognized as a person who is part of a family and a community not just a patient number in a study.” The researchers say that at each part of the process, from developing studies to reporting the results back to the community, they have learned invaluable lessons. Mittleman said, “Community-based research allows you to ask questions that you can’t ask any other way, and you need the answers for the science. But the questions don’t have easy, short answers, so you have to be involved for the long haul.”
Back to Top
Nutrition Research Day shares new territory explored by clinical research dietitians
 |
Several Nutrition Research Day participants interact during a break in the panel presentations.
|
The Clinical Center Nutrition Department on March 18 hosted their annual research day, which drew dietetic interns from across the region as well as participants from across the country in a week-long CC-NCI nutrition and cancer prevention research practicum. Representing all levels of training, from undergraduate to Ph.D., the approximately 75 attendees learned about the role of clinical research dietitians at the CC and a sampling of nutrition-related protocols.
Nancy Sebring, clinical research dietitian, told the group how CC dietitians often serve as associate investigators for many clinical research protocols. Currently more than 75 protocols at the CC require specific nutrition research services, such as research diets, body composition measurements, dietary and eating behavior assessments, interpretation of metabolic studies, and nutrition counseling or classes.
During the parade of examples of nutrition-related protocols, clinical research dietitians shared their experiences in areas ranging from developing a low iodine diet to supporting a sleep intervention study. For many studies, the dietitian’s challenge may be to keep the patient nourished throughout and after treatment by translating the dietary changes required by the protocol or disease into food choices the patient can make in daily life. Jennifer Graf, who discussed a natural history protocol for Progeria Syndrome, a disease of premature aging, said the rewards of working as a dietitian in clinical research include exploring new clinical territory, discussing parameters of new treatment protocols, and interacting with patients.
 |
Merel Kozlosky, director of the NIH dietetic internship and supervisory metabolic dietitian, welcomes the attendees.
|
Nutrition as a field is also increasingly involved in the cutting-edge territory of biomedical informatics, which Dr. James Cimino, chief of the new Laboratory for Informatics Development, defined in his presentation as the art and science of organizing knowledge of human health and disease, and making it useful for problem solving. Madeline Michael, chief of clinical nutrition services in the Nutrition Department, described the CC’s experience transforming practice from paper to electronic health records and designing nutrition documentation for research. Dr. Amy Subar, a nutritionist with NCI, shared how her team developed an automated, self-administered 24-hour dietary recall system. By answering a series of questions about what they ate, patients create a food list of what they consumed the day before that—with further probing about food preparation, additions, and portion size—leads to the assignment of a standard USDA food code that is used to calculate a total nutrient and food group intake for the reporting day.
Afternoon breakout sessions included tours of the CC, NLM, and the Metabolic Clinical Research Unit and presentations on botanical and other dietary supplements and assessing dietary intake with food frequency questionnaires. Research Day is organized by the NIH dietetic internship director. Merel Kozlosky, who is in her first year in the position, said “the looks of awe and enlightenment on the faces of the dietetic interns, nutrition students, and professionals was very rewarding and inspiring.”
Back to Top
CC staff reflect on women's art, vision
 |
|
(from left): CC music therapist Shelia Egan, CC Chief Operating Officer Maureen Gormley, and CC art therapist Megan Robb. Gormley gave the opening remarks and moderated the commemorative event, while Robb gave the keynote speech and Egan led an interactive presentation on music therapy.
|
Three Clinical Center staffers shared their insights at the March 19 NIH Women’s History Month observance.
Giving the keynote presentation, Megan Robb, an art therapist in the recreation therapy section of the CC Rehabilitation Medicine Department, shared how art therapy—which she described as a women-dominated field drawn from women’s intuitive strengths—can help people heal, resolve conflicts, develop interpersonal skills, manage behavior, reduce stress, and improve self-esteem and awareness.
CC music therapist Shelia Egan described how she creates a moment of normalcy in abnormal situations by using music to bring CC patients and families to a more centered place.
Back to Top
Wound care exhibits answer staff questions
 |
|
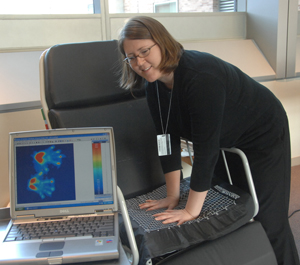
Laurie DeLaney, an occupational therapist and assistive technology practitioner with the CC Rehabilitation Medicine Department, demonstrates the department's pressure mapping system. It evaluates pressure distribution in wheelchairs and beds and shows patients and nurses areas at risk for pressure ulceration.
|
One of the eight issues the Clinical Center's multidisciplinary quality improvement committee chose to emphasize for 2008 is wound care and pressure ulcer prevention.
For three days in February Karen Chandler Axelrod, the CC’s wound, ostomy, and continence nurse specialist, and ICU nurse Linda Tondreau co-coordinated exhibits for ICU staff in the third floor bridge area focusing on bed education, pressure ulcer prevention, ostomy teaching, and skin care.
 |
|
(from left): Karen Chandler Axelrod, wound, ostomy, and continence nurse specialist, shows ICU nurse Julissa Reyes information about pressure ulcers.
|
Axelrod and Tondreau also will co-coordinate a larger exhibit for the entire CC on April 30. The event will bring in the reps of products used at the CC giving the nurses, nurse practitioners, physicians, and physicians’ assistants an opportunity to stop by and learn about the products directly from the reps and the ICU staff who frequently use the items. “The staff say they really would like to learn more,” she said.
Back to Top
News Briefs
 |
The logo for National Medical Laboratory Professionals Week
|
CC departments celebrate Lab Week
National Medical Laboratory Professionals Week, April 20-26, is a time to honor the more than 280,000 medical laboratory professionals across the nation who perform and interpret laboratory tests that save lives and keep people healthy. Several Clinical Center departments—including the Department of Laboratory Medicine, the Department of Transfusion Medicine, and Pathology—are celebrating the work of their laboratory professionals, including pathologists, laboratory technologists, phlebotomists, and technicians. Using state-of-the-art technology and instrumentation, laboratory staff help to prevent disease by detecting unknown health problems and by aiding in the diagnosis and treatment of existing conditions by giving accurate, timely test results. Doctors rely heavily on lab tests to make diagnoses, thus laboratory professionals are critical components of the health care system. Results of laboratory tests often identify the presence of disease in its earliest stages, when the possibilities of a cure are greatest and when treatment is least costly.
First annual NIH career symposium
On April 9 the Graduate Student Council, NIH Fellows Committee, the Foundation for Advanced Education in the Sciences, and the Office of Intramural Training & Education will sponsor the first annual NIH career symposium. The event allows NIH graduate students, as well as postdoctoral and clinical fellows, to explore the diverse careers a science education makes possible. Interactive panel session topics include science policy and education careers; career options for clinicians; and employment in public and private sectors. Experts from diverse educational and career backgrounds—from MDs working in pharmaceuticals to PhDs working in patenting—are represented on 15 different panels. The event also features workshops on professional skills, including leading a team and networking. During lunch and an afternoon reception, trainees can meet and network with panel speakers. For more information, visit www.training.nih.gov/symposium.
Walk with CC patients on their journey of hope
The Clinical Center seeks community volunteers to serve as patient ambassadors. Opportunities are available Monday to Friday, 6 a.m. to 8 p.m. Volunteers will accompany patients in wheelchairs to appointments within the CC, as well as transport items critical for timely patient care, such as medical records. Relevant training for working within a hospital environment will be provided. A minimum commitment of one year and 200 hours is requested. For more information, come to an open house on Wednesday, April 16 at 6:30 p.m. in the atrium or Tuesday, April 29 at 2 p.m. on the 1SE patio, call 301-496-2642, email ambassadors@cc.nih.gov or see www.cc.nih.gov/volunteers
Back to Top
New clinical research protocols
The following new clinical research protocols were approved in February:
Phase I Study of Bortezomib and Cetuximab without or with Cisplatin in Combination with Radiation Therapy for Advanced Head and Neck Cancer, 08-C-0071, Carter Van Waes, MD, NCI
A Phase II Study of Satraplatin and Prednisone in Metastatic Androgen-Independent Prostate Cancer (AIPC), 08-C-0074, William L. Dahut, MD, NCI
Phase III Evaluation of Recombinant MAGE-A3 Vaccine as Adjuvant Therapy Following Resection of MAGE-A3-Positive Non-Small Cell Lung Cancer, 08-C-0075, David S. Schrump, MD, NCI
A Phase I, Multi-Institutional, Open-Label, Dose-Escalation, Multiple Dose Study of the Safety, Tolerability, and Immune Response of CRS-207 in Adult Subjects with Selected Advanced Solid Tumors Who Have Failed or Who Are Not Candidates For Standard Treatment, 08-C-0077, Raffit Hassan, MD, NCI
A Phase I/II trial of Pemetrexed (Alimta [Registered Trademark]) Combined with Sirolimus (Rapamycin, Rapamune [Registered Trademark]) in Subjects with Relapsed or Refractory NSCLC Whose Tumors Bear Activation of mTOR, 08-C-0078, Phillip A. Dennis, MD, NCI
Natural History Study and Longitudinal Assessment of Children, Adolescents, and Adults with Neurofibromatosis Type 1, 08-C-0079, Brigitte C. Widemann, MD, NCI
SARC Global Collaboration: A Phase II Trial of R1507, a Recombinant Human Monoclonal Antibody to the IGF-1 Receptor for the Treatment of Patients with Recurrent or Refractory Ewing's Sarcoma, Synovial Sarcoma, Rhabdomyosarcoma and Other Sarcomas, 08-C-0080, Lee J. Helman, MD, NCI
Registration Phase III Study of Lucanix (TM) (Belegenpumatucel-L) in Advanced Non-Small Cell Lung Cancer: An International Multicenter, Randomized, Double-Blinded, Placebo-Controlled Study of Lucanix(TM) Maintenance Therapy for Stages III/IV NSCLC Subject, 08-C-0083, Giuseppe Giaccone, MD, NCI
Identification of Biomarkers in Exhaled Breath Condensates from Asthmatic Patients, 08-H-0081, Stewart J. Levine, MD, NHLBI
Evaluation of Systemic Toxicity Associated with Allogeneic Peripheral Blood Stem Cell Infusion, 08-H-0084, Courtney D. Fitzhugh, MD, NHLBI
fMRI Investigation of Cortical Reorganization and Phantom Limb Pain Following Amputation, 08-M-0052, Christopher I. Baker, PhD, NIMH
Back to Top
Upcoming Events
April 2, 2008
Ethics
Conflicts of Interest and Peer Review: What Ought To Be Done?
Arthur Caplan, Ph.D.
Emmanuel and Robert Hart Professor of Bioethics
Chair, Department of Medical Ethics, and Director, Center for Bioethics, University of Pennsylvania
Lecture will be videocast, http://videocast.nih.gov
April 9, 2008
Great Teachers
Mysterious Cases
Gurpreet Dhaliwal, M.D.
Assistant Clinical Professor of Medicine, University of California, San Francisco
Lecture will be videocast,
http://videocast.nih.gov
April 16, 2008
Systems Biology of Diabetic Nephropathy
Robert G. Nelson, M.D., Ph.D.
Staff Clinician, Phoenix Diabetes Epidemiology and Clinical Research Branch, NIDDK
Matthias Kretzler, M.D.
Associate Professor, Division of Nephrology/Internal Medicine, Computational Medicine and Biology, University of Michigan
April 23, 2008
Clinical Manifestations and Treatment of H5N1 Avian Influenza Infections in Humans
John Beigel, M.D.
Staff Clinician, Laboratory of Immunoregulation, NIAID
Epidemiology and Prevention of H5N1 Avian Influenza Infections
Kanta Subbarao, M.D., M.P.H.
Senior Investigator, Laboratory of Infectious Diseases, NIAID
April 30, 2008
Complications of Rheumatoid Arthritis
Michael W. Ward, M.D., M.P.H.
Investigator, Office of the Clinical Director, Intramural Research Program, NIAMS
SNPs, Chips, and Autoimmunity: New Frontiers in the Genetics of Rheumatoid Arthritis
Elaine F. Remmers, Ph.D.
Staff Scientist, Genetics and Genomics Branch, NIAMS
Back to Top
This page last updated on 12/14/2017


 The information on this page is archived and provided for reference purposes only.
The information on this page is archived and provided for reference purposes only.