July 2016
IN THIS ISSUE:
![]()
- Wayfinding app helps navigate the Clinical Center
- 35 Years of HIV/AIDS: Dr. Anthony Fauci reflects on past, pushes toward future actions
- Staff try virtual reality equipment, learn about its potential for research
- NIH Blood Bank plays crucial role for stem cell transplant recipient
- Attention Federal Employees: HHS Launches Demographic Survey – Online Only
- National Symphony Orchestra performs Peter and the Wolf
- Project SEARCH at NIH graduates sixth class, five interns hired on as feds
- What's wrong when nothing seems to be wrong? Lecture highlights functional disorders
- Three nurses honored in May for leadership – Online Only
- Volunteers needed for NIAID study on conditions that cause inflammation – Online Only
- Safety, Health & Wellness Day features screenings, exhibits, tastings and more – Online Only
Print this Issue ![]() (285 KB)
(285 KB)
ABOUT CC NEWS:
![]()
Published monthly by the Office of Communications and Media Relations. News, article ideas, calendar events, letters, and photographs are welcome. Submissions may be edited.
Clinical Center News
National Institutes of Health
Building 10, 10 Center Drive
Room 6-2551,
Bethesda, MD 20892-1504
Tel: 301-594-5789
Fax: 301-402-0244
Molly.Freimuth@nih.gov
2016 ISSUES:
![]()
QUICK LINKS:
![]()
Wayfinding app helps navigate the Clinical Center
 A free application called NIHCC Take Me There is now available to help individuals find their way around the Clinical Center. The tool can pinpoint current locations and provide directions to nearly anywhere in Building 10 and can be accessed by smartphone devices and a website.
A free application called NIHCC Take Me There is now available to help individuals find their way around the Clinical Center. The tool can pinpoint current locations and provide directions to nearly anywhere in Building 10 and can be accessed by smartphone devices and a website.
The app can be downloaded on iOS [disclaimer] and Android devices [disclaimer]. The website allows users to share directions with others via email or print, an important feature for international visitors or patients without smartphone devices.
"This initiative can aid safety, operational efficiency, and improve patients' and visitors' overall experience," said Dr. John I. Gallin, director of the Clinical Center.
This initial release of the app includes features such as:
- The Directory allows users to browse for locations like clinics, departments, and points of interest, as well as search for and find NIH Staff. Profiles provide descriptions and contact information.
- My Places allows users to add and store 'Favorites'- both locations and staff.
- Parking Planner is a tool for patients and visitors pre-planning their visit, and My Car enables users to save parking locations.
- Points of Interest can be searched in the directory or via the map.
- Navigation is driven by user position and provides turn-by-turn directions, graphic route instruction, including the directional arrow and real-time user positioning in the form of a blue dot, which is accurate to 2-3 meters and refreshed every second.
- The Staff Filter enables filtered searches for staff from the NIH directory.
- Housekeeping, created to report housekeeping, maintenance and facility related issues, allows users to submit the location of the incident, description and/or images.
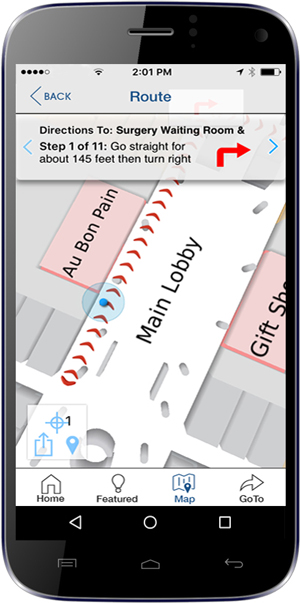 The app, which includes a Spanish-language version, works in the hospital's common or public areas, but not within private office suites such as those in the north side of the building.
The app, which includes a Spanish-language version, works in the hospital's common or public areas, but not within private office suites such as those in the north side of the building.
"A small cross-departmental group of Clinical Center staff worked tirelessly on this new tool, constantly shaping features with the comfort and needs of our patients as the foremost priority," said Gallin.
The effort was led by Eric Cole, director of the Office of Administrative Management, with primary support from the Office of Communications and Media Relations, and assistance from the Hospitality Department and Department of Clinical Research Informatics. Dr. Robert Balaban, the scientific director of the Division of Intramural Research (DIR) at the National Heart, Lung, and Blood Institute (NHLBI), expressed the initial need for more navigational support. Eva Sarbah-Yalley, a nurse on the 5th floor inpatient units, is behind the creation of the wayfinding app's name.
"Already, a number of other hospitals have caught wind of this initiative and are seeking to learn from our experience," added Gallin.
Questions? Contact eric.cole@nih.gov
![]()
35 Years of HIV/AIDS: Dr. Anthony Fauci reflects on past, pushes toward future actions
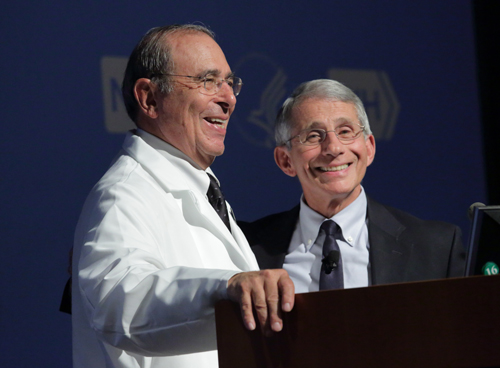 |
Dr. John I. Gallin, director of the NIH Clinical Center, and Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), at the June 5 Grand Rounds. |
On June 5, 1981, just 35 years ago, the Centers for Disease Control and Prevention reported the first five cases of what is now known as acquired immunodeficiency syndrome (AIDS) in the U.S. Human immunodeficiency virus (HIV), if left untreated, is what attacks cells in the body's immune system and advances to AIDS.
In 1982, less than a year since the initial reports were published in the Morbidity and Mortality Weekly Report (MMWR), hundreds of additional reports of other patients with AIDS were being published and congressional representatives took action to introduce legislation funding NIH to conduct AIDS research. Scientists at NIH and around the world were soon studying a disease about which they knew nothing – but had the foresight to know it would be a life changing field of medicine.
Almost to the day of the 35th anniversary of the MMWR report, Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), reflected on decades of HIV/AIDS research and current vaccine trials and preventative methods during a Clinical Center Grand Rounds lecture titled AIDS at 35: Is the End in Sight?. He presented a call to action to end the HIV/AIDS epidemic.
"The end is indeed in sight, but there is a lot that we still need to do to get to that end," Fauci said. "If you look at the U.S., there is a degree of complacency because of the fact that we have good treatment. But we really still have a major problem."
Youths 13-to-24-years-old account for 22 percent of newly diagnosed HIV infections, he added. In addition, Fauci added that men who have sex with men along with African Americans bear the greatest burden of HIV.
"In the U.S., if you are a gay man and African American, there is a 1 in 2 chance that you will have HIV infection in your lifetime. That is an unacceptable health statistic that is true. We do really have a major challenge."
In front of 500 lecture attendees in Masur Auditorium and 400 people watching live via videocast, he said that the best path forward in HIV/AIDS research and for a decrease in the epidemic, will be by following the science.
"It is the science that has been accomplished by the scientific community, by many of you in this room, and many countless colleagues throughout the country and the world that has brought us to the point where we can actually say, maybe, if we implement the science,...maybe the end is in sight. Over the 35 years of science at NIH and in medical centers throughout the world there has been nothing short of breathtaking scientific advances."
One of the most pivotal discoveries, made in 1994, through a NIAID sponsored clinical trial, was a new drug combination that helped patients sustain undetectable viral loads. A viral load refers to the amount of HIV in the blood. Patients with undetectable viral loads still have HIV, but are able to live longer, healthier lives and have a reduced risk of HIV transmission.
Prior to the development of these antiretroviral drugs, which prevent HIV from replicating, the life expectancy for a 20-year-old newly diagnosed with HIV in the 1980s was roughly 12 years. Today, on antiretroviral medication, that number has jumped to roughly 52 years. There are 17 million people globally on antiretroviral therapy.
"The screening for the first effective drug that gave us the treatment we have was from individuals right in this building," Fauci stated.
For patients with HIV, there are treatment and prevention options that work. And the foundation for treatment and prevention is HIV testing. If someone is tested positive, then there's a care continuum for treatment, to save his/her own life and prevent the infection of anyone else. But just as important is for those who don't test positive to maintain in the HIV prevention continuum with health care providers.
"If you just test everybody who's infected and put them in care, you will decrease 91.5% of all the infections in the United States," Fauci stated. There's a global target of 90-90-90. "If you get 90% of the people [who have HIV but haven't been tested] diagnosed, and of those you put 90% on treatment, and of those, you virally suppressed 90% — if you do that, you wind up with 73% of all the infected people in the world virally suppressed. That turns around the trajectory of the epidemic."
Resources & More Information
Historical Reflections from NIH Clinical Center Leaders |
![]()
Staff try virtual reality equipment, learn about its potential for research
 |
Lindsay Lauren, a summer fellow with the National Institute of Child Health and Human Development, was one of 60 staff members who participated in the virtual reality demonstration in the Clinical Center. |
At the NIH, researchers are looking at ways to use virtual reality to help experts advance their science and allow patients to practice for conditions they may face in the real world.
On June 16, Noah Robinson, a Postbaccalaureate Intramural Research Training Awardee within the NIH Clinical Center Rehabilitation Medicine Department, held an all-day demonstration of the virtual reality equipment.
With the simple pulling of the mask over the eyes, a person can be immersed into a carefully controlled environment that is generated by a computer.
During the demonstration, visitors were able to practice working in an office environment or cooking in a kitchen. In a research hospital setting, the environment shown through virtual reality can then be easily modified according to how the participant responds – and can get them up and moving through physical exercise. Patients with functional limitations can also feel empowered as they explore new surroundings. Treatments can be individualized by allowing the system to monitor physiological responses such as heart rate through a fitness tracker and manipulate the presentation of stimuli in real time.
This ability to change things quickly and easily for a patient is one of the things that Robinson says is great about virtual reality.
"Virtual reality unlocks the ability for us to immerse subjects in any environment we can think of. There is tremendous creativity available to design environments that are not possible in real life," he said. "It is customizable, and the barrier to learn how to build environments is low."
During the demo, he showed NIH staff how to easily build new virtual environments and use downloaded 3-D graphics for any situation. The equipment is relatively inexpensive and can be built on a typical PC.
Robinson, who left at the end of June to pursue his Ph.D. in clinical psychology at Vanderbilt University, said that he really wanted to demonstrate to staff that you have to experience virtual reality firsthand to see the potential on how it can be used in science. He has been working for two years on using virtual reality in the NIH Clinical Center Rehabilitation Medicine Department with patients who have Parkinson's disease and those who have Cerebral Palsy. In the future, after his experience at NIH, Robinson hopes to conduct clinical research through a free Internet-based clinical intervention for those with depression and anxiety.
And, while Robinson has left the NIH, there are many others who are interested in continuing to incorporate virtual reality into their research. The virtual reality interest group, which has about 75 members, helps people start using the technology and share ideas. For more details on the group, email varig@list.nih.gov.
![]()
NIH Blood Bank plays crucial role for stem cell transplant recipient
 |
Pediatric patient Sophia Trujillo (front row) recently visited the NIH Donor Center at Fisher’s Lane in Rockville to thank them for their support and care. From left to right (back row), Dr. Anne Eder, Hal Wilkins, Daniel Llenas, Sherry Smoot, Earlene Thompson, Celina Montemayor, Natasha Hammond, Michelle Trujillo, Juan Salgado and Cathy McGraw. |
On May 25, staff at the NIH Donor Center at Fisher's Lane in Rockville, Md., received a special visit from 7-year-old Sophia Trujillo, a patient whose treatment at the NIH Clinical Center, along with blood donations from the Donor Center, saved her life.
Sophia arrived at the NIH in October 2015, desperately in need of a bone marrow transplant to treat her aplastic anemia. Aplastic anemia, a rare blood disorder, didn't allow her bone marrow to make enough new red blood cells, white blood cells and platelets. Her blood was unable to clot, and her immune system was left defenseless.
Despite a worldwide search on Be The Match [disclaimer], a national bone marrow registry, Sophia could not find a matching donor amongst the 27 million potential people listed. So, she turned to NIH.
Sophia and her mother Michelle traveled from Chicago to join a clinical trial in the National Heart, Lung, and Blood Institute (NHLBI), led by Dr. Richard Childs, a Senior Investigator in the Laboratory of Transplantation Immunotherapy, and a Rear Admiral in the U.S. Public Health Service Commissioned Corps. A mismatched unrelated umbilical cord blood unit combined with stem cells from her mother, who was only a partial tissue match, were used during the transplant. To prepare Sophia for the transplant, she was given chemotherapy and other treatments to wipe out her entire immune system to prevent rejection of the transplanted cells. On February 10, 2016, Sophia received her brand new immune system – an IV infusion of thawed cord blood stem cells combined with highly purified stem cells from Michelle.
Despite the joyous milestone, Sophia still had a long journey ahead. Typically, it takes more than 100 days until Childs and his team are able to tell if the stem cells have permanently engrafted – meaning the patient's body has accepted the transplanted bone marrow and started to make healthy blood cells.
But often, complications arise.
In January, Sophia's nearly non-existent immune system couldn't protect her from a fungal infection that was located in her eye. The infection was so critical that her medical care team knew they had to act quickly, otherwise Sophia would lose her eyesight.
She needed the help of granulocytes – white blood cells that fight infection.
Despite the blizzard conditions outside, NIH staff trekked in to prepare Michelle for her donation of granulocytes. Unlike other blood donations that can take place in one day, donating granulocytes is a bit more physically- and time-intensive.
"White blood cells are only viable for 24 hours," said Hal Wilkins, Recruitment Supervisor in the Department of Transfusion Medicine. "They require the donor to come in the day before for medication to increase the amount of white blood cells in the circulatory system. Then, the donor must come in the next day for the actual donation. Only people who are enrolled in a special protocol can donate. Currently we have 67 participants, and we need so many more."
Within 40 minutes of transfusion of granulocytes, "Sophia's eye became swollen and purple. The granulocytes went straight to the site fighting the infection," Michelle said.
 |
Pediatric patient Sophia Trujillo and one of her care providers, Celina Montemayor, look at equipment used to collect blood at the NIH Donor Center at Fisher's Lane in Rockville. |
The normal number of white blood cells in the blood is 4,500 to 11,000 white blood cells per microliter.
"Her white blood cell counts went from 200 to 16,000 after my granulocytes," Michelle added.
Over the next few weeks, Sophia needed seven more granulocyte infusions from other donors.
"As a parent, to know that seven additional people came in to step up to save a life, it's just amazing," Michelle said.
During her treatment at the NIH Clinical Center, Sophia also received 66 platelet donations, which are small cells that help the blood clot – 52 of which were pathogen-reduced to best prevent any possibility of infection in the recipient. And, she was given 20 units of regular blood donations, roughly equivalent to 20 pints.
"A lot of people contributed to this miracle," Wilkins said during Sophia's visit to Rockville. "This is the outcome everybody would be praying for, and it's all because of the research, the staff, the volunteers and the donors. They all came together to have a miracle like Sophia."
"It puts everything in prospective of what we do here," added Juan Salgado, apheresis supervisor at the NIH Fishers Lane Donor Center. Salgado was able to meet Sophia and her mom during their visit. Salgado, along with colleague Natasha Hammond, drove to work in the January blizzard to ensure that Michelle could donate granulocytes to Sophia.
Overwhelmed with joy, Michelle thanked Sophia's team at NIH and those at the NIH Donor Center at Fisher's Lane.
"Without the medical team, without the granulocytes, that infection would have caused a different ending," she said. "I made the best decision to come out to NIH. It's hard as a parent, you don't want to say it, but if we were anywhere else I feel that she wouldn't have made it."
Sophia has recently surpassed Day 100 post-transplant. Inspired by her time at NIH and her doctor, Sophia has big plans that may one day lead her back to the Clinical Center.
"I want to be a doctor like Dr. Childs, because he's an admiral, and he helps people with aplastic anemia and makes them feel better," Sophia said.
Learn more about how to donate blood.
![]()
Attention Federal Employees: HHS Launches Demographic Survey – Online Only
HHS launched a Department-wide survey on July 20 to update Federal employee records on race, ethnicity and disability status. The Office of Management and Budget (OMB) and the U.S. Census previously updated the categories for race and ethnicity, and HHS is conducting this survey to ensure that we have accurate and up to date demographic information for employees within the Department.
Currently, NIH and other agencies within the department do not have updated information for employees who were onboard prior to the changes in the OMB and Census standards. These changes include the ability to identify with more than one racial category, separation of the Asian and Pacific Islander racial categories, addition of a racial category for Native Hawaiian and Other Pacific Islanders, and the option to identify ethnicity (Hispanic/Latino) and race.
In addition to providing an opportunity to update demographic data for the workforce and correct any errors that may exist in the database, the survey will also provide an opportunity to update the disability status of employees. Employees may develop disabilities throughout the course of their careers that did not exist when they entered the workforce.
This information is imperative as HHS benchmarks the workforce against the available labor pool, and develops strategies to recruit and retain a diverse and inclusive workforce. Additionally, having an accurate count of the number of employees with disabilities and the types of disabilities prepares HHS to identify and provide effective accommodations.
Federal employees will receive an email from HHS with a link to the survey. The survey is housed in the Access Management System's (AMS) secure environment. Please take five minutes to participate in this voluntary survey to ensure that HHS has an accurate demographic data for the workforce. Questions about the survey should be sent to PiSurvey@hhs.gov.
![]()
National Symphony Orchestra performs Peter and the Wolf
On June 22, in the Clinical Center atrium, patients, visitors and staff were dazzled by the Russian composer Sergei Prokofiev's musical tale, Peter and the Wolf, presented by The National Symphony Orchestra (NSO). The visit marked its 16th NIH concert as part of its Sound Health initiative. The story was narrated by Lesli Foster (seen above), a reporter from WUSA Channel 9 News. View WUSA's coverage of the event [disclaimer] (Note: The concert marked the NSO's 16th visit to the NIH Clinical Center, not the 14th year as reported.) |
![]()
Project SEARCH at NIH graduates sixth class, five interns hired on as feds
 |
The sixth class of Project SEARCH at NIH interns gather at the NIH Clinical Center before a graduation celebration June 3. Back row, left to right: Monique Walters, William Calvert, Gabriel Leder, Damien West, Alec Callahan and Trevon Womack. Front row, left to right: David Han, Lisa Katz, Valerie Riguax, Maurine Yap and Sabrini Babu. |
Eleven young professionals in the Project SEARCH-NIH program graduated June 3 in the Clinical Center, after completing 30 weeks of vocational education and training. The program, which began at NIH in 2010, prepares those with intellectual and developmental disabilities for competitive employment opportunities. Five interns were hired after completing the program, four within the federal government and one as a contractor.
Since 2010, 69 interns have graduated and 41 have been hired at the NIH. More than 90% of those who were hired by the NIH are still employed in their position. And, in total, six graduates who were hired in the community are still employed in their positions.
Participants complete rotations throughout the Clinical Center and other areas on the NIH campus, performing important tasks that help them build job skills. In this graduating class, participants had the responsibility to change out medical records in an outpatient clinic, locate and decal hospital equipment as well as other tasks in maintenance, IT and food services sections.
Several graduates worked with Donna Phillips, director of the Division of Facilities Operations and Maintenance in the NIH Office of Research Facilities. At the graduation ceremony, Phillips praised the program and the graduates and said their hard work has made a real impact at NIH. The graduates working within Phillips office helped identify and locate inventory valued at over $50,000.
David Han, a 2016 Project SEARCH-NIH graduate, said that while at NIH he especially cherished the opportunity to "learn to grow in the community." Also, one of his favorite administrative tasks was helping plan of patient discharge schedules.
Trevon Womack, another graduate, said that he also enjoyed being a part of the NIH community and participating in events such as Take a Hike Day. Womack stated that his confidence grew during his time in Project SEARCH-NIH.
![]()
What's wrong when nothing seems to be wrong? Lecture highlights functional disorders
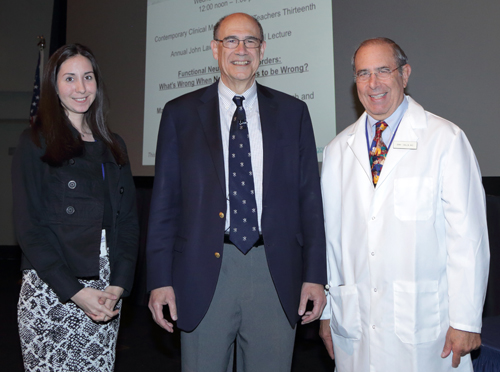 |
Dr. Mark Hallett (center), chief of the Medical Neurology Branch at the National Institute of Neurological Disorders and Stroke, gathers with Dr. Cemre Robinson (left), a co-chair of the NIH Fellows Distinguished Clinical Award Selection Committee, and Dr. John I Gallin (right), director of the NIH Clinical Center. |
On June 8, Dr. Mark Hallett, chief of the Medical Neurology Branch at the National Institute of Neurological Disorders and Stroke, presented the 13th Annual John Laws Decker Memorial Lecture on the topic of "Functional Neurological Disorders: What's Wrong When Nothing Seems to be Wrong?" Hallett is the recipient of the 2015 NIH Distinguished Clinical Teacher's Award (DCTA), an honor bestowed on an NIH senior clinician, staff clinician or tenure-track/tenured clinical investigator by the NIH clinical fellows.
"I've always felt that one of the greatest awards that you can receive here at NIH is the Distinguished Clinical Teacher's Award," said Dr. John I. Gallin, director of the NIH Clinical Center. The memorial lecture honors the legacy of Dr. John Laws Decker who served as NIH Clinical Center director from 1983 to 1990. "What's more important than getting recognition from the fellows, who are tomorrow's leaders?"
Addressing a full crowd in Lipsett Amphitheater of colleagues, fellows and other trainees, Hallett discussed functional movement disorders as examples of functional neurological disorders. The disorders often prove difficult to diagnose and involve involuntary movements such as a spasm or tremor.
"What's wrong with these patients? Their usual neurology work up is normal, MRI/EEG, blood tests – everything seems to be fine," Hallett stated. "This has led to the common phrase one hears, that 'these patients don't have real disease.' But they do have real disease, and there must be something wrong with them. So, I thought, we better take this on as one of our responsibilities in the laboratory, and we've had this as one of our major areas of research for over the past 20 years."
Hallett outlined the differential diagnosis of functional movement disorders, including conversion disorder, the main topic, factitious disorder and malingering. Conversion disorder, as named by Dr. Sigmund Freud, and once referred to as "hysteria," is a disorder where a person unconsciously produces movements presumably resulting from a psychological disorder. Factitious disorder is a medical illness where similar movements are produced voluntarily, and malingering is not an illness, but when people pretend to be sick as a way to achieve a secondary goal, such as obtaining drugs or disability benefits. Factitious disorder and malingering and both rare.
The cause of conversion disorders is still uncertain, but there is an understanding that biology, social environment and psychology all play a role. There are no gene mutations definitively linked to these disorders. Early life stress, even while in utero, may play an important role in potential causes. The stress could lead to changes in the brain.
 |
Hallett discussed functional movement disorders as examples of functional neurological disorders in front of a full crowd in Lipsett Amphitheater. |
In the brain, humans not only have the intention to move their body but also the ability to make the decision to move – before movement is generated. In patients with functional neurological disorders, over-activation of the brain's limbic system, which controls emotion and behaviors, might lead to an abnormal intention to move and decision to move.
There is also a mechanism in the brain that creates ownership of the movement, once the movement has been completed. Humans make a decision to move, and then the brain takes credit for that movement. In patients with functional neurological disorders, the mechanism is dysfunctional, leading to involuntary movements over which patients do not have ownership.
Hallett hopes his team's continued research can help educate all health care professionals so that patients can be better diagnosed.
"This is a problem for all fields of medicine," said Dr. Hallett. "There is more to do and understand, but we are making progress."
![]()
Three nurses honored in May for leadership – Online Only
|
![]()
Volunteers needed for NIAID study on conditions that cause inflammation – Online Only
NIAID study seeks healthy adult volunteers, 18-64 years old. Researchers want to better understand the effects of glucocorticoids on the body. These medications are commonly used to treat conditions that cause inflammation on the skin and in the body like lupus, asthma, and eczema. This research may help us to find better treatments for people with conditions that cause inflammation. Participants will receive one intravenous dose of a glucocorticoid, and a glucocorticoid cream will be applied to a small area of the skin. Blood and skin samples will be collected. Two outpatient visits at the NIH Clinical Center are needed. Compensation is provided. (Study #16-I-0126)
For more information on the study above or others available, call the NIH Office of Patient Recruitment 1-866-444-2214, (TTY 1-866- 411-1010) or visit www.clinicaltrials.gov.
![]()
Safety, Health & Wellness Day features screenings, exhibits, tastings and more – Online Only
 On June 22, the NIH Clinical Center hosted the 2016 NIH Safety, Health and Wellness Day in the South Lobby. Safety, Health and Wellness Day serves to reach out to all NIH staff in an effort to enhance employee nutrition, wellness, physical fitness and safety awareness and to reduce work-related injuries and illnesses. The event included health screenings, physical fitness activities and classes, safety and health promotion exhibits and nutrition demonstrations and tastings.
On June 22, the NIH Clinical Center hosted the 2016 NIH Safety, Health and Wellness Day in the South Lobby. Safety, Health and Wellness Day serves to reach out to all NIH staff in an effort to enhance employee nutrition, wellness, physical fitness and safety awareness and to reduce work-related injuries and illnesses. The event included health screenings, physical fitness activities and classes, safety and health promotion exhibits and nutrition demonstrations and tastings.
 This annual event was sponsored by the Office of Research Services, Office of Research Facilities, NIH Occupational Safety and Health Committee, IC Safety Chairpersons Committee, Laboratory Sustainability Group, and 2016 IC co-sponsor, the National Institute of Allergy and Infectious Diseases.
This annual event was sponsored by the Office of Research Services, Office of Research Facilities, NIH Occupational Safety and Health Committee, IC Safety Chairpersons Committee, Laboratory Sustainability Group, and 2016 IC co-sponsor, the National Institute of Allergy and Infectious Diseases.
More information about employee health and safety.
NOTE: PDF documents require the free Adobe Reader.



