CC pediatric program receives grant that helps expand CAH research
 |
Dr. Deborah Merke (right) is able to see more patients like Zachary Ward (center) because of funding
|
Two foundations are helping expand NIH research into the rare disease Congenital Adrenal Hyperplasia (CAH).
Dr. Deborah Merke, chief of pediatric services for the Clinical Center, has received more funding for her natural history protocol of CAH.
The non-profit CARES Foundation (Congenital Adrenal Hyperplasia Research Education and Support) is continuing its funding of Merke’s research with a $50,000 grant from the family foundation Peregrine Charities.
CARES began funding CAH research at the Clinical Center in 2005. Merke is using the money to include nurse practitioner Carol Van Ryzin on the research team. Having a nurse practitioner dedicated solely to CAH clinical research has been invaluable,” says Merke. “It allows us to see more patients with CAH and to start new clinical research studies that otherwise would not have been possible.”
CAH is a group of inherited disorders that affect the adrenal gland. The most severe form, classic CAH, is usually detected shortly after birth or in early childhood and can be life threatening. The milder form, nonclassic CAH, causes a variety of symptoms that may appear anytime from infancy to adulthood. Some common symptoms are: premature development of body hair; an early rapid growth spurt but short stature as an adult; severe acne; anxiety and depression; and infertility.
Merke is leading a natural history study of patients with CAH. The study, sponsored by NICHD, will chronicle aspects of development over several years. Researchers want to learn which physiological processes are affected by the disease and why. The information could help scientists design treatments that would address the underlying problems rather than just the symptoms.
The CARES funding has helped Merke see so many more patients (101 in a nine-month period) that she is able to expand the research and collaborate with other institutes at NIH.
Merke’s team is working with Drs. Monique Ernst and Daniel Pine in NIMH to study the psychological aspects of hormonal imbalances. The team also is collaborating with Dr. Nazli McDonnell, NIA, to look at other genes that may influence CAH symptoms and their severity.
Merke’s work already has made a difference in people’s lives and demonstrated the need for more research and education. The clinical research team here found that four of the 101 patients had been misdiagnosed before they came to the Clinical Center. The four had conditions that were not CAH and had been taking drugs they did not need. One of those study participants was a child with a tumor in his testicle. Merke referred the child for treatment and says he is now cured.
“This indicates how misunderstood CAH is,” Merke says. “That’s the reason we need to expand our understanding of the disease, but also educate physicians so the disease is not misdiagnosed in the future.”
The CARES foundation is a non-profit organization that helps people affected by CAH. Peregrine Charities is a grantmaking family foundation formed to help families afflicted by rare or “orphan”diseases that affect fewer than 200,000 people nationwide.
—Shana Potash
Back to Top
New contingency hospital enhances emergency response
 |
Capt. Elaine Ayres inspects contingency hospital inventory
|
September 11, 2001, was a major impetus for the emergency-response partnership formed in 2004 by the NIH Clinical Center and its neighbors, National Naval Medicine Center and Suburban Hospital. The Clinical Center’s role in the partnership was tested during last year’s hurricane Katrina, when the hospital’s capacity flexed to accommodate about 100 patients from the Gulf Coast region.
The need wasn’t realized, but the preparations were a real-life test of the hospital’s capability to accept an influx of patients. Accommodating such a surge is a major role for the CC under the partnership. Navy and Suburban can transfer or divert certain types of patients to the CC so incoming sick and injured can receive care at the facility best suited to provide it.
“The partnership hospitals have complementary strengths,” said Dr. John I. Gallin, CC director. “The NIH Clinical Center has physicians who represent almost every medical and surgical specialty and subspecialty. Naval Medical Center staff are skilled and trained to respond to all kinds of emergencies and Suburban Hospital is a level II trauma center.”
DHHS recognized the partnership’s potential early on—it’s the only such collaboration that includes hospitals from the private, government and military sectors—and earmarked a 250-bed contingency hospital for its support. The contingency hospital comprises pre-positioned supplies and equipment for ready set up within the Clinical Center. This ‘within the walls’ deployment is both practical and unique, noted Dr. David K. Henderson, the CC’s deputy director for clinical care and liaison for the partnership. “We have space to put the beds and staff from throughout NIH who have volunteered to provide the care.”
Again, Katrina intervened. CC was to have received the nation’s first of 10 such pre-positioned hospitals. Supplies and equipment being assembled in Atlanta were redirected to areas affected by the hurricane, explained Capt. Elaine Ayres, project officer for the contingency hospital.
It took months, but the CC’s contingency hospital—200 containers covering 3,000 square feet—has now been reassembled, delivered and stored. “The inventory, tailored to supplement what we already have at the CC, allows us to be self-sufficient for at least 72 hours,” said Ayres. If the hospital is activated in response to an emergency, staff here will simply unpack the 200 containers and set up the beds, equipment and supplies in pre-determined areas throughout building 10.
 |
Clinical nurse specialists Beth Price and Ann Peterson greet CC staff volunteers representing a surge of incoming patients during a recent drill.
|
The boxes are color coded, meticulously inventoried and precisely arranged to simplify logistics. They include everything from beds for patients and cots for staff to IV poles and blood pressure cuffs.
There are no pharmaceuticals and few supplies that can’t be stored indefinitely, she said. Ayres, CC assistant director for ethics and technology development, was the PHS team leader for another contingency hospital sent to Mississippi in the aftermath of Katrina and staffed by NIH volunteers. The experience, she added, provided invaluable insight into how such resources can best be set up and used.
The members of the Emergency Preparedness Partnership will stage their third preparedness drill in December. The previous exercises provided opportunities to practice and refine response processes under fairly realistic circumstances. “Our goal is to be flexible and creative in our response to emergencies,” Henderson said.
Back to Top
Weingart explores the anatomy of error in fellows’ rounds
“Humans err,” said Dr. Saul N. Weingart, vice president for patient safety and director of the Center for Patient Safety at Dana-Farber Cancer Institute. “Training, communicating, and reminding are weak interventions,” said Weingart in a sweeping analysis of medical error, in a Grand Rounds lecture for clinical fellows last month. “Only by probing deeply can we understand the conditions that lined up to allow something unfortunate to happen. You’ve got to change the system.
“Don’t rely on memory or vigilance,” said Weingart, “or expect people to perform well when fatigued.” Simplify routines, reduce handoffs, build in redundancies and provide better information. Create forcing functions (making it impossible to do action B without precondition A). Make use of best practices—bar coding, for example, and repeating verbal orders.
Recognize missteps for what they are. Cognitive psychologists recognize three models of error in human performance: skill-based, rule-based, and knowledge-based. Human factor scientists call skill-based errors slips and rule-based and knowledge-based errors mistakes.
Skill-based behavior is rapid, effortless, and unconscious—things you do automatically, such as brushing your teeth, buttoning your shirt, driving to work. Characteristic slips involve
• Capture (you’re supposed to do one sequence of steps, A,B,C,F, and instead you do A,B,C,D, because A,B,C,D is more common—as when you load up the family car for vacation and absentmindedly drive toward the office)
• Description error (correct action, wrong object—pouring syrup in your coffee or milk on your pancakes)
• Associative activation (having the wrong cue trigger a particular behavior—the doorbell rings and you answer the phone)
• Loss of activation (striding purposefully into a room and not remembering why you are there).
“These slips are common across all cultures,” says Weingart. “They are part of the human phenotype.” We’re built to perform many functions on an unconscious level so that we can think about other things that are more interesting and important. “But those automatisms allow us to get into trouble. And they are degraded by the things you’d expect, such as fatigue, illness, alcohol, sleep deprivation, and boredom.”
Rule-based behavior (when it’s raining, take an umbrella) is important in medical training. Using mnenomics, we train physicians in rule-based behaviors with code algorithms, said Weingart. “The trick is to apply it in the correct setting.” Rule-based mistakes occur when we apply the wrong rule—for example, going down a code algorithm but choosing the wrong arm.
Knowledge-based behavior involves solving novel problems, coming at them afresh. Knowledge-based mistakes, of which there are many, have to do with biased memory and intellectual convenience. We like to use the solution we used last time, or we don’t like to change our mind once we’ve come up with an initial hypothesis, or we’re overconfident about what we decide.
Knowing we are faulty machines and that errors are inevitable, said Weingart, we must design medical care systems that make those errors transparent and reduce the number of preventable adverse events and close calls. It’s important, says Weingart, to take care of yourself, take care of the system, and reduce blame and shame. “If we’re not free to talk about errors,” he said, “we’ll never learn from them."
—Pat McNees
Back to Top
Principles, practice of clincal research course registration set
Registration for the 2006-2007 Introduction to the Principles and Practice of Clinical Research course is open through Oct. 6. The course runs Oct. 16, 2006, through Feb. 20, 2007. Classes will be held on the NIH campus on Monday and Tuesday evenings, 5 p.m. to approximately 6:30 p.m. There is no charge for the course. The textbook, Principles and Practice of Clinical Research, is suggested as supplemental information for the course. A certificate will be awarded upon successful completion of the course, including a final exam.
Close to 800 students registered for the 2005-2006 program, which was also broadcast to several domestic and international locations. For additional information or to register, please go to the course website, http://www.cc.nih.gov/researchers/training/ippcr.shtml or call the CC Office of Clinical Research Training and Medical Education, 301-496-9425. An e-mail confirmation will be sent to those accepted into the program.
Back to Top
Patients come first
 |
Ramon Rodriguez
At the Clinical Center for 35 years
Job: Housekeeping leader
Housekeeping and Fabric
Care Department
|
Ramon Rodriguez has a simple formula for success, which has earned him friendship, admiration and respect over the years. “Pay attention. Do the work. If something needs to be done, do it.”
In his current job, Rodriguez is a critical link in his department’s innovative program for cleaning patient rooms and treatment areas. He ensures delivery of the small, water-conserving microfiber mops—lightweight, efficient, and easy to clean and maneuver —now used throughout the CC. In patient care areas, a clean mop goes to each room, every shift. The CC was one of the first hospitals to adopt this approach, a system that cuts the risk of cross-contamination between rooms and speeds cleaning because staff no longer have to empty and refill large buckets of water. No more old-fashioned mop buckets means fewer worker injuries.
Rodriguez, who worked many years as a housekeeper in patient-care units, estimates he covers a couple of indoor miles every workday, plus “three miles outside before work, because I have to be in shape.”
Fluent in Spanish, Rodriguez always has a kind word for patients who seem worried, or humor when a laugh is in order. “The patients remember my jokes,” he says, smiling.
“It’s a nice place to work,” he said. “People are friendly and work together.”
Back to Top
Dr. Jaffe receives the 2006 Distinguished Clinical Teacher's Award
 |
Dr. Elaine Jaffe (center), NCI, receives the 2006 Distinguished Clinical Teacher’s Award and is congratulated by CC Director John I. Gallin (left) and award committee chairperson Dr. NaYong Kim, NIAID.
|
NCI’s Dr. Elaine Jaffe received the 2006 Distinguished Clinical Teacher’s Award, the highest honor bestowed on an NIH senior clinician, staff clinician, or tenuretrack clinical investigator by the NIH Clinical Fellows.
The award was presented Sept. 6 at the first Clinical Center Grand Rounds of the 2006-2007 academic year.
Recipients of the award, given annually since 1985, are recognized for their excellence as a mentor and teacher and their contributions to clinical research.
Dr. NaYoung Kim, NIAID fellow, chaired this year’s award committee and read a few comments from fellows as she introduced Jaffe. “Fellows are in awe of her amazing clinical skills, and there is often a sense that we are in the presence of greatness as she teaches the intricacies of diagnosis while signing out clinical cases at the microscope,” was one. Another tribute: “Whenever clinicians have questions or want to discuss issues surrounding patient care, Dr. Jaffe stops whatever she is doing and devotes her undivided attention to the clinical team to help manage difficult clinical issues.”
Jaffe joined the NCI as a resident in anatomic pathology and has been a senior investigator since 1974. Her current area of expertise is in the molecular basis of lymphoma and the use of targeted inhibitors to develop more effective treatments for cancer.
As the 2006 DCTA award recipient, Jaffe will deliver the Fourth Annual John Laws Decker Memorial Lecture during a NIH Clinical Center Grand Rounds in June 2007.
“Mentors have always played a key role in the professional life of physicians,” Dr. John Gallin, CC director said at the start of the presentation. “And, outstanding clinical mentors have certainly been an important part of the Clinical Center’s success for more than 50 years.”
The finalists for the 2006 DCTA award were Drs. Jeffrey Cohen (NIAID), Barry Gause (NCI), Phillip Dennis (NCI), Sandra Swain (NCI), and Neal Young (NHLBI).
Back to Top
CC gallery exhibits a special blend of art and science
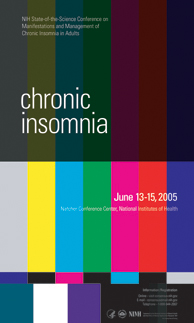 |
Designer Bryan Ewsichek created this award-winning poster in 2005 to promote the NIH state-of-the-science conference on the manifestations and management of chronic insominia in adults.
|
Their job is to tell the story of NIH research. They do it eloquently and in great detail. And, they do it with few, if any, words.
For decades, medical illustrators and graphic designers with NIH Medical Arts have contributed to the understanding and awareness of advances made by researchers at NIH.
A new exhibit, which is on display in the Clinical Center galleries until Nov. 3, showcases this special blend of art and science. The exhibit, “NIH Medical Illustrations and Poster Design Past to Present,” features a collection of medical illustrations from the 1950s to the present and a retrospective of posters created for scientific conferences and other events.
“I think our posters and medical illustrations should be the best in the country because we represent the country in the field of health care,” says lead illustrator Alan Hoofring. “We should push the envelope and set a look that everyone else wants to achieve.”
“The medical illustrators at NIH are phenomenal artists,” says Lillian Fitzgerald, curator of the Clinical Center galleries.
“Their illustrations are an integral aspect of our research and part of the fabric of NIH,” adds Crystal Parmele, director of the CC art program.
The exhibits celebrate the collaboration between artist and researcher, and provide an interesting window on how both science and the visual arts have progressed during the past 60 years.
Illustrations in the exhibit represent a range of topics and artistic styles and show the evolution of approaches from hand-drawn to computer-aided and three-dimensional renderings.
Hoofring’s 2004 entry is a medical journal illustration explaining the story of the barriers encountered when attempting to deliver drugs to the interior of the eye. It is a pencil sketch combined with imaging-editing software. There is an incredible amount of information per square inch in the artwork.
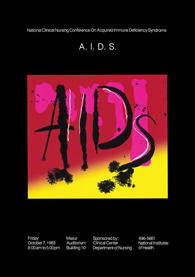 |
This AIDS nursing conference poster was created in 1983 by Betty Hebb, former Medical Arts staffer.
|
At the other end of the style spectrum is a bold and bright computer-aided rendition of an essential metabolic enzyme, pyruvate dehyrdrogenase, by Don Bliss, now with the National Library of Medicine. The artwork created for cancer research made the cover of a medical journal in 2002.
The illustrators and designers, past and present, say while the tools they use have evolved, the bigger changes are the subjects they are asked to represent. These artists are doing fewer anatomy and surgery pieces and more illustrations of research at the molecular level.
“We follow the science,” explains Linda Brown, creative director for NIH Medical Arts. “It’s cutting-edge. The procedures are experimental. The science is new. It gives us the opportunity to do things that no one else gets to do.”
And, they frequently do it first—illustrating topics that haven’t been illustrated before.
One example is the AIDS research in the 1980s, says Martha Blalock, team lead design and illustration for NIH Medical Arts. “When scientists first started researching the virus that causes AIDS, we didn’t know what it looked like. Illustrators were coming up with these new images. We’re capturing memories and pieces of a period of time in scientific development.” The exhibit includes one of the first posters for an AIDS conference.
“We’re a very rare breed. There aren’t many of us running around,” says Bartner, describing the unique service illustrators provide and the specialized, graduate-level training. Bartner worked at NIH for 42 years before retiring in 2000. A sample from his extensive body of work is included in the exhibit.
“We’re not illustrating birds and flowers. We’re illustrating information that may need clarification and will be further enhanced with images,” explains Bartner. September 2006 Clinical Center news continued from page 4 A good illustrator, he says, “can take the ideas, and photos, or whatever a doctor brings to your desk, and create an image that goes far beyond what the doctor anticipated.” A good illustrator creates pieces “that are beautiful to look at and pull you into the drawing so you come away understanding something you might not have understood before.”
The illustrators and graphic designers at NIH all say the key is to listen, to understand just what’s in the head of the person who asked for help.
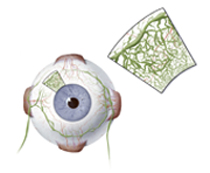 |
Alan Hoofring won an American Medical Illustration Award of Excellence for this work explaining the barriers encountered when trying to deliver drugs into the eye.
|
 |
A computer-aided rendition of the essential metabolic enzyme, pyruvate dehydrogenase was created by Don Bliss, former staffer. The image made the cover of the European Medical Biology Organization (EMBO) journal.
|
Three current medical illustrators, Hoofring, Ethan Tyler and Lydia Kibiuk have won prestigious American Medical Illustration awards. All three, and several past illustrators, graduated from the training program at Johns Hopkins School of Medicine, where they took anatomy, cell biology, histology, and other courses alongside medical students. All three took a class at Hopkins from an outstanding illustrator at NIH, Howard Bartner.
Graphic designers are called upon to create the posters, invitations, mailers and other collateral for lectures and special events, and to produce public education and patient recruitment materials.
Designer Bryan Ewsichek says it’s his job to take in a lot of information and distill it into something the public understands. “It comes down to the simplest image to tell the story for the general public—an image that is eye catching and will draw people in.” The exhibit includes a poster he created for a conference on chronic insomnia. He based his design on a television test pattern one would see in the early morning hours when all programming has ended and most people have gone to sleep. The poster earned him an award from the American Institute of Graphic Arts and the honor of being published in Communication Arts 2006 Design Annual, a prominent graphic design magazine.
Hoofring and Blalock, who organized the exhibit, say this is a chance for the artists to honor their clients. As Bartner notes, “the relationships you form with the doctors enhances your experience.” There’s no other experience like NIH says Brown, “Where else do you get to sit at a table and talk with a Nobel Prize winner and watch him fold up a napkin to explain the image he wants you to create.”
The exhibit in the NIH Clinical Center runs through November 3. The illustrations are on display on the first floor of the Hatfield building. The posters can be seen on the first floor of the Magnuson building. For directions and additional information, please visit, http://medarts.nih.gov.
—Shana Potash
Back to Top
New policy for fingernails, hand hygeine approved
 |
There’s a new hand-hygiene policy for health-care workers at the Clinical Center. It’s based on guidelines the CDC published in 2002 and tailored to the CC environment. Important information includes:
Fingernails. Artificial nails or natural nails longer than a quarter inch above the fingertip are not allowed. This applies to health-care workers involved in the direct care of high-risk patients or those who have contact with aspects of the care of high-risk patients, such as food, medications or sterile equipment.
Hand hygiene requirements. Hand hygiene (using soap and water or alcohol hand gel) must be performed by every health-care worker:
• At the beginning and at the end of each shift.
• Before and after every patient contact.
• Before handling or preparing food or eating.
• After using the restroom or changing diapers.
• Before donning gloves for direct patient contact or sterile procedures.
• When moving from a contaminated body site to a clean body site during patient transport
• Before performing an invasive procedure.
• After removing personal protective equipment (e.g., gloves).
• After contact with blood, body fluids or other potentially infectious materials, even if hands are not visibly soiled.
• After touching objects that are likely to be contaminated with microorganisms (for example, equipment or other items in a patient room, keyboards, telephones, doorknobs).
• When hands are soiled (for example, after sneezing, coughing or blowing your nose).
The complete policy, approved by the Medical Executive Committee in June, is online, http://internal.cc.nih.gov/policies/PDF/M06-2.pdf
Back to Top
CC staffer specializes in sax, clarinet, databases
 |
Chris Epinger plays the saxophone regularly for weddings, memorials and church services.
|
“Music creates order out of chaos,” said acclaimed violinist Yehudi Menuhin, “for rhythm imposes unanimity upon the divergent, melody imposes continuity upon the disjointed, and harmony imposes compatibility upon the incongruous.”
Do computers help tame information in a similar fashion? Maybe, and maybe that’s one reason musicians—including Chris Epinger, database and Web administrator for the Clinical Center—are well represented in the field. Epinger plays sax and clarinet, and many of his co-workers are also musicians.
Epinger planned to be a musician after graduating from the Hartt School of Music, in Connecticut, and as a member of the musicians’ union he played for jazz bands and pit orchestras. But those jobs don’t pay the mortgage, so he took a low-level job as a computer operator for a firm in West Hartford, “got the bug,” and figured he might make a career out of it.
Does musical ability prepare one for computer programming? “Funny you should ask that,” says Epinger. That first firm sent him for training to a computer processing institute, and when he told them he was a musician they said that was perfect for programming. “I was kind of skeptical about that,” says Epinger, “but I seem to be able to pick up programming concepts quickly, so they may be right. It uses the same part of the brain, apparently. And I’ve known a lot of musicians who have now gone into the computer science field and have done very well.”
Epinger was visiting a college friend in Washington when he spotted an ad for a computer job at the Kennedy Center, which sounded ideal for a musical computer guy. He got the job, handling everything from desktop support to telecommunications and database administration, but after 15 years and three executive directors decided it was time to try something else. For four years he’s worked happily in the CC’s Department of Clinical Research Informatics. “It’s much nicer being part of a large department,” he says, “because you don’t have to do everything yourself.”
Camaraderie and collaboration typify his musical avocation, too. One of Epinger’s favorite annual gigs is a British “music hall” (variety show) performance with the British Embassy Players. He plays regularly with a group called the Associates (former colleagues at the Kennedy Center), swing, dance band, and classical music, often for friends’ weddings, commitment ceremonies, memorials, or church services. What he enjoys most is reading through standard jazz charts or show music with friends, playing around with it, and varying the rhythm, style, or interpretation. “You can do this on your own practice time,” says Epinger, “but it’s better with other people because you play off each other’s ideas.”
When colleagues found out about his tuneful avocation, they were amazed that the Computer Guy could be a musician.
—Pat McNees
Back to Top
Fellows on board for clinical, translational research training
Thirty medical students representing 19 schools from around the country have been selected for fellowships in the 2006-2007 Clinical Research Training Program (CRTP) for Medical and Dental Students at NIH. The recipients, who have completed clinical rotations at their home institutions and will work in the Clinical Center, arrived late summer to begin 12 months in clinical and translational research training in their chosen field. This is the program’s tenth year.
The training program, established in 1997 with nine fellows, provides creative, research-oriented medical and dental students with an opportunity to become involved with and learn about clinical research early in their careers. Since 1998, the program has been supported jointly by the NIH and the Foundation for the National Institutes of Health through grants from Pfizer Inc as part of the company’s commitment to public-private partnerships. The partnership included 15 students annually starting in 1998. In 2004, the program was expanded to accept 30 students a year thanks to support through the NIH Roadmap as part of its Re-engineering the Clinical Research Enterprise initiative.
“NIH’s Clinical Research Training Program offers medical and dental students a remarkable foundation for their involvement in clinical research as their careers progress,” said Dr. Elias A. Zerhouni, NIH director.
One hundred and sixty students who represent the next generation of clinician scientists have participated in the program to date. A committee of established clinical researchers at the NIH reviews and makes selections based on applications received from qualified medical and dental students around the country. This year’s recipients were selected from a field of 80 applicants.
Simply described, the goal of NIH research is to acquire new knowledge to help prevent, detect, diagnose, and treat disease and disability, from the rarest genetic disorder to the common cold. The NIH mission is to uncover new knowledge that will lead to better health for everyone, and providing learning opportunities for students is a critical to encouraging future science and scientists.
“While at NIH, the fellows are paired with a renowned investigator as a mentor,” noted Dr. Frederick P. Ognibene, CRTP director. “These clinician-scientist mentors are individuals who are making groundbreaking discoveries and moving scientific knowledge from the bench to the bedside. During the year-long experience the students learn the principles of clinical research, write a research protocol, and conduct either clinical or translational research alongside some of the most prominent researchers in the world today,” he said. “It’s an experience that would be hard to replicate elsewhere. In my six years as director, I have been uniformly impressed that the CRTP has been a life-changing and career-enhancing experience for its participants.”
Back to Top
Upcoming Events
October 3 Tuesday
7 p.m., Masur Auditorium
Medicine for the Public: Stroke Update
Steven Warach, M.D., Ph.D.
Chief, Stroke Diagnostics and Therapeutics
Section, NINDS
October 4 Wednesday
12 noon- 1 p.m., Lipsett Amphitheater
Ethics Rounds: Condemning Contraception
Conversations in Consent
Margaret Little, Ph.D
Associate Professor of Philosophy
and Senior Research Scholar, Kennedy Institute
of Ethics, Georgetown University
Carol Bayley, Ph.D.
Director of Ethics and Justice Education,
Catholic Healthcare West
October 10 Tuesday
7 p.m., Masur Auditorium
Medicine for the Public:
Tuberculosis in the 21st Century:
Old problem, New Understanding
Steven M. Holland, M.D.
Chief, Laboratory of Clinical Infectious Diseases,
NIAID
October 11 Wednesday
12 noon- 1 p.m., Lipsett Amphitheater
Contemporary Clinical Medicine Great Teachers
Parables and Pearls: Interesting Cases in the
Management of Hematologic Malignancies
Eric Seifter, M.D.
Associate Professor of Medicine and Oncology
Johns Hopkins University School of Medicine
October 17 Tuesday
7 p.m., Masur Auditorium
Medicine for the Public: The Role of the Gut,
Hormones and the Brain in Obesity
Monica C. Skarulis, M.D.
Chief, Clinical Endocrine Section,
Clinical Endocrinology Branch, NIDDK
October 18 Wednesday
No Grand Rounds
NIH Research Festival
For more information, go online
http://researchfestival.nih.gov
October 24 Tuesday
7 p.m., Masur Auditorium
Medicine for the Public: AIDS After 25 Years:
Lessons Learned For Other Emerging Infections
Henry Masur, M.D.
Chief, Critical Care Medicine Department,
Clinical Center
October 25 Wednesday
12 noon- 1 p.m., Lipsett Amphitheater
Sixth Annual John Doppman Memorial Lecture
for Imaging Sciences
MRI-Guided Focused Ultrasound Surgery
Ferenc A. Jolesz, M.D.
B. Leonard Holman Professor of Radiology;
Vice Chairman for Research; Director, Division
of MRI and Image Guided Therapy Program,
Department of Radiology; Brigham and Women’s
Hospital; Harvard Medical School
October 31 Tuesday
7 p.m., Masur Auditorium
Medicine for the Public: Depression:
Impact, Causes, and Current Research
Peter Schmidt, M.D.
Chief, Unit on Reproductive Endocrine Studies,
Behavioral Endocrinology Branch, NIMH
Back to Top
News Briefs
Plan now to foil the flu
The influenza vaccine for the 2006-2007 season contains the following strains recommended by the FDA’s Vaccines and Related Biological Products Advisory Committee: A/New Caledonia/20/99 (H1N1), A/Wisconsin/67/2005 (H3N2) andB/Malaysia/2506/2004. Look for the upcoming schedule in the next CCNews and online, http://www.foiltheflu.nih.gov/. If you have questions about the influenza vaccine, call the Clinical Center Hospital Epidemiology Service, 301-496-2209.
Physical Therapy Month events
October is National Physical Therapy Month. The theme is “Moving You to Better Health.” with a focus on: “Bike Right, Bike Fit.” Meet staff at the entrance of the second floor cafeteria on Wednesday, 11 a.m. to 1 p.m. on Oct. 11 to kick off the celebration. A representative from the NIH Bike Club will offer information on proper bike fit and posture On Oct. 27, 8:30-9:30 a.m., come to room 4-2551 for a presentation by Cynthia Zadai of the Massachusetts General Hospital Institute of Health Professionals. Her topic is “Current Concepts of Mobility Management for Inpatients with Cardiovascular Dysfunction."
Doppman lecture
Dr. Ferenc A. Jolesz of Harvard Medical School and Brigham and Women’s Hospital will present the sixth annual John Doppman memorial lecture for imaging sciences at 12 noon on Oct. 25 in Lipsett Amphitheater. His topic is “MRI-Guided Focused Ultrasound Surgery.”
Back to Top
Clinical Center News, National
Institutes of Health, Building 10, 10 Center Drive, Room 12C440, Bethesda, MD 20892-1504. Tel: 301-496-6787.
Fax: 301-402-2984. Published monthly for CC employees
by the Office of Communications, Patient Recruitment, and Public Liaison. News, article ideas,
calendar events, letters, and photographs are welcome.
Back to Top
|
|


 The information on this page is archived and provided for reference purposes only.
The information on this page is archived and provided for reference purposes only.